PALS Renewal: Who Needs It & When
If you’re an RN, respiratory therapist, pharmacist, or allied health provider, maintaining Pediatric Advanced Life Support (PALS) certification is often a job requirement. The American Heart Association (AHA) designed PALS specifically for healthcare providers involved in the management of critically ill infants and children. These include professionals in emergency rooms, pediatric intensive care units, anesthesia, trauma teams, and prehospital systems.
You need to renew your PALS card every two years. The certification remains valid until the last day of the expiration month shown on your card. Employers typically track these deadlines closely, and in most cases, your ability to participate in clinical care depends on maintaining a current certification.
Letting your card lapse can disqualify you from taking the shorter renewal course. Most AHA training sites do not allow a grace period. If your card has expired, you’ll likely need to retake the full provider course. That course involves more time, cost, and preparation compared to the renewal path.
The safest approach is to begin planning your renewal six months before expiration. Doing so gives you scheduling flexibility and helps avoid gaps that could impact your shift assignments or hospital credentialing.
Prerequisites & Essentials Before You Enroll
Before enrolling in a PALS renewal course, you must meet several important requirements. The most essential is that your existing AHA PALS certification must still be valid on the day of your renewal class. If it has expired—even by one day—you may be required to take the full provider course instead.
Most training centers also require you to hold a valid Basic Life Support (BLS) certification. Since BLS is a foundation for all advanced life support techniques, the AHA emphasizes that participants must already be proficient in its use. You may be asked to present both cards on arrival, and some programs check this during registration.
You’ll also need access to the most current PALS Provider Manual and reference cards. These resources include algorithms, pediatric dosage charts, and structured assessment guides. They’re often available in both print and eBook formats, and some courses include them in the fee. If not, purchasing them in advance is highly recommended.
Equally important is the Precourse Self-Assessment (PSA), a mandatory online quiz that tests your baseline knowledge. You’ll need to complete it before attending your hands-on session. Most programs require a minimum passing score of 70% and request that you bring proof of completion. The PSA covers rhythm identification, pharmacology, and general PALS principles. It helps ensure that everyone attending the renewal class arrives ready for team-based simulation.
Format & Structure of PALS Renewal for Healthcare Providers
PALS renewal is available in two formats: the traditional instructor-led class and the HeartCode® blended learning path. Both paths culminate in a hands-on testing session with live instructors.
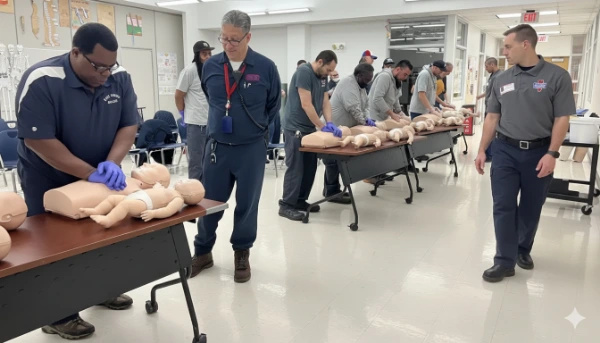
In the instructor-led model, you’ll attend a one-day, in-person class. The course typically runs 6 to 8 hours depending on class size, scenario complexity, and retesting needs. You’ll rotate through pediatric emergency stations, participate in team-based simulations, and demonstrate critical skills like BLS, IO access, defibrillation, and medication administration.
The HeartCode option starts with an online adaptive learning module. This module uses scenario-based activities to tailor your learning experience. After completing the online portion, you’ll schedule a skills session with a certified instructor. The hands-on part usually lasts 3 to 4 hours and includes scenario practice and testing.
Both paths include a final team-based “megacode” simulation. Instructors evaluate your ability to manage respiratory failure, bradycardia, tachycardia, cardiac arrest, and shock in pediatric patients. These scenarios require active communication, clinical decision-making, and precise adherence to PALS algorithms.
Here’s a simplified chart of the two main renewal options:
| Format | Online Time | In-Class Time | Skills Testing Required | Notes |
|---|---|---|---|---|
| Instructor-led | None | 6–8 hours | Yes | Most common for hospitals |
| HeartCode (blended) | 4–6 hours | 3–4 hours | Yes | Flexible for shift workers |
Role-Focused Prep: What RNs, RTs, and Allied Health Should Emphasize
Different provider roles require different clinical focuses, and your PALS preparation should reflect that. As an RN, concentrate on medication administration, rhythm recognition, and fluid resuscitation. You’ll likely serve as a team leader, documenter, or medication nurse in scenarios, so precision in dosing and timing is essential.
Respiratory therapists should emphasize airway management and ventilation strategies. Practice using bag-valve-mask devices on infants and children. Understand when to escalate to supraglottic airways or endotracheal intubation. Also, review troubleshooting for ventilator settings in pediatric emergencies.
Pharmacists and other allied professionals should focus on dosing calculations, drug sequences, and algorithm transitions. Know when to use epinephrine, amiodarone, or adenosine and how to adjust doses based on weight. Rehearse the “Pediatric Assessment Triangle” to rapidly categorize patients into respiratory distress, failure, or shock categories.
Regardless of your role, rehearse closed-loop communication and role delegation. PALS scenarios depend on seamless teamwork, and confusion during simulations often leads to point deductions or failures. Practice vocalizing findings, confirming orders, and rotating roles under pressure.
This chart outlines the core clinical priorities for each major healthcare role participating in PALS renewal. Use this to fine-tune your study plan based on your professional focus.
| Provider Role | Primary Focus Areas | Secondary Emphases |
|---|---|---|
| Registered Nurse (RN) | Medication administration, IV/IO access, rhythm recognition, bradycardia vs tachycardia protocols | Leading teams, documenting interventions, rapid reassessment strategies |
| Respiratory Therapist (RT) | Pediatric airway management, BVM technique, ventilation strategies for respiratory failure | Endotracheal confirmation, oxygen titration, PEEP adjustment in children |
| Allied Health (Pharmacist, Techs) | Dose calculation, drug prep/sequence, use of code carts and checklists | Contributing to debriefs, helping track timing, equipment logistics |
Performance Metrics & Course Updates to Note
Since the 2020 guideline update, the AHA has placed a stronger emphasis on objective performance metrics during resuscitation scenarios. One major addition is the use of real-time feedback devices during CPR to monitor depth, rate, and recoil. These devices ensure that your compressions meet the recommended standards.
A key metric is Chest Compression Fraction (CCF), which is the percentage of time compressions are delivered during cardiac arrest. PALS instructors now aim for a CCF greater than 80%, meaning minimal interruption in chest compressions.
Another recent focus is the CPR Coach role. This designated team member provides compression feedback and announces countdowns for compressor switches. Evidence shows that having a CPR Coach improves outcomes and adherence to AHA benchmarks.
The 2020 guidelines also updated ventilation rates when an advanced airway is present: 1 breath every 2–3 seconds, totaling 20–30 breaths per minute. This reflects the unique needs of pediatric patients with high respiratory demands.
Finally, the guidelines reinforce the early administration of epinephrine, ideally within 5 minutes of cardiac arrest recognition. Providers should now prioritize early vascular access and dose readiness to meet this target.
These 2020 AHA guideline updates frequently appear in renewal scenarios and skill stations. Knowing them helps you avoid outdated practices and testing pitfalls.
| Topic Area | 2020 Guideline Change | Implication for PALS Renewal |
|---|---|---|
| CPR Quality | Use of real-time feedback devices to guide compressions | You may be evaluated on depth, recoil, and rate in live testing |
| Chest Compression Fraction (CCF) | Target CCF ≥ 81% during cardiac arrest | Avoid long pauses during rhythm checks or role switches |
| CPR Coach Role | New designated team role to ensure CPR quality and transitions | You may be assigned this role in testing scenarios |
| Advanced Airway Ventilation | New rate: 1 breath every 2–3 seconds (20–30/min) | Breath timing must align with new rate during megacode |
| Epinephrine Timing | Administer within 5 minutes of starting compressions | Delays may result in scenario failure or point loss |
Renewal Logistics: From Testing to Certification
During your skills test, instructors will assess your ability to perform BLS for infants and children, manage airways, interpret rhythms, and execute pharmacologic interventions. You must perform these within the correct sequence and under time constraints.
Scenarios often include cases of respiratory arrest, bradycardia with poor perfusion, supraventricular tachycardia, pulseless arrest, and distributive or cardiogenic shock. Each provider will rotate through different roles, and teamwork is key.
Retesting is sometimes allowed if you fail a station, but policies vary. If your course includes a retest opportunity, instructors will typically give immediate feedback and allow a second attempt during the same session.
Come prepared with the following:
- Current PALS and BLS cards
- Completed Precourse Self-Assessment (printed or saved)
- Valid photo ID
- A pen and notepad for note-taking
- Comfortable scrubs or clothing for manikin work
After passing, your AHA eCard is issued within 24 to 48 hours. Some training centers will email you a direct link; others require you to claim it via the AHA’s website.
Common Pitfalls & Practical Tips for Success
One of the most common mistakes is arriving without a completed Precourse Self-Assessment. Even if you’ve done the review online, forgetting the proof can delay your participation. Always print or digitally save your results.
Another error is assuming your BLS or PALS card is still valid when it’s actually expired. Double-check the expiration date and register for your renewal before the deadline.
Communication failures can sink an otherwise strong team. Avoid vague commands, and always use closed-loop confirmation. For example, say “Give 0.01 mg/kg epinephrine IV push now,” and expect a full verbal confirmation.
Lack of rhythm practice is another issue. Spend time reviewing narrow-complex tachycardia, bradycardia, ventricular fibrillation, and asystole. You should know what to do without consulting the manual.
Arrive early on test day. Rushing leads to anxiety, forgotten items, and poor performance. Aim to be calm, focused, and well-rested.
Sample Study Plans for Nurses, RTs, Allied Professionals
A structured four-week plan works well for most busy providers:
- Week 1: Review the PALS Provider Manual. Focus on algorithms, CPR sequences, and team roles.
- Week 2: Practice ECG rhythm strips. Use apps or flashcards to quiz yourself on patterns and interventions.
- Week 3: Simulate scenarios at home or with coworkers. Focus on teamwork, timing, and communication.
- Week 4: Review drug cards and dosing charts. Rehearse rapid calculations and sequence timing.
Nurses should drill medication prep and delivery using realistic scenarios. Respiratory therapists should practice rapid airway transitions using airway manikins or props. Allied professionals can benefit from focused review of pharmacology and scenario transitions.
Use mobile-friendly tools like AHA’s PALS apps or rhythm simulators. These allow for 10-minute practice sessions between shifts or during downtime.
What Happens if Your Card Expires?
If your certification expires, you usually cannot attend a renewal course. AHA policy states that only current cardholders may take renewal options. Many institutions follow this rule strictly.
Expired cards may force you to attend the full two-day provider course again. That option involves more extensive preparation, higher tuition, and additional clinical scenarios.
Avoid this by setting a reminder 90 days before your expiration. Schedule early, and always verify course dates to align with your availability. Don’t assume you’ll be able to walk in last minute.
Course Provider & Scheduling Considerations
Always verify that your training provider is AHA-certified. This ensures your eCard is valid and recognized by employers and credentialing bodies.
Class slots for renewal can fill fast—especially before license renewal periods or at the end of the year. Register early and confirm cancellation or refund policies.
Ask whether course fees include the manual, reference cards, and online access codes. Some providers itemize these separately.
Plan your commute and parking ahead of time. Know the building layout, start time, and check-in procedures. Bring food and water if breaks are short or offsite food is unavailable.
If you work nights or rotating shifts, pick a class that aligns with your body clock. Fatigue can impair both cognitive and physical performance during scenarios.
Next Steps Toward Renewal Readiness
Make your checklist and confirm every detail. Your PALS card, BLS card, PSA results, ID, and manual should all be in hand before class day.
Arrive early and settle into the environment. Quietly review your algorithm cards, especially bradycardia, arrest, and shock.
Use breaks to mentally rehearse role rotations. If allowed, team up with classmates during scenarios for smoother transitions.
After class, promptly claim your AHA eCard via the provided link. Download it as a PDF for employer credentialing. Log your CE units in your state licensing portal or internal HR system.
Keep your PALS knowledge fresh with periodic reviews, especially if you don’t regularly encounter pediatric emergencies. Simulation drills, team practice, and short-form refreshers keep your skills sharp and ready for real-world emergencies.
