Key Takeaways
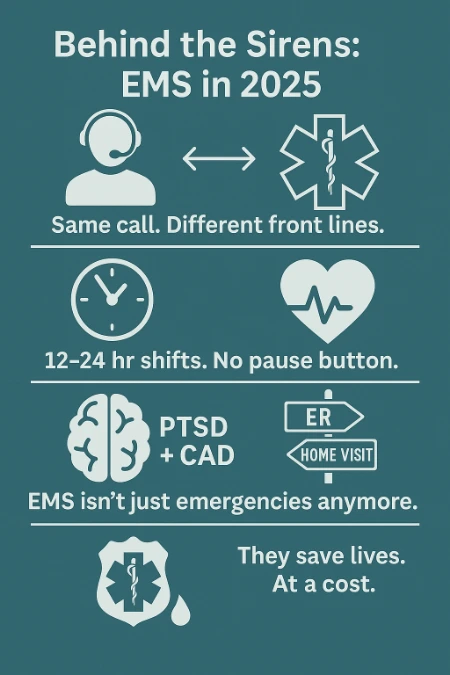
- EMS professionals in 2025 face expanding responsibilities beyond emergency response, including chronic care and mental health intervention.
- The job’s emotional and physical toll—burnout, PTSD, and cardiovascular risk—remains high and often unaddressed.
- Real stories from dispatchers, paramedics, and community medics reveal a profession driven by compassion, resilience, and evolving public expectations.
A Profession Defined by Urgency, Compassion, and Chaos
Why EMS Work in 2025 Is More Complex Than Ever
EMS professionals now handle far more than just trauma calls or cardiac arrests. Their role bridges emergency medicine, social services, and public safety. Rising call volumes and complex patient needs stretch crews thin across cities and rural areas. Many EMS teams now manage overlapping duties like documentation, mental health crises, and chronic illness support. These added pressures demand sharper decision-making skills and deeper emotional resilience.
From 911 Calls to Care Coordination: The Expanding EMS Role
In 2025, EMS responders do much more than transport patients to hospitals. Many now coordinate home-based care plans with community health teams. During one shift, a paramedic might manage a stroke call, then provide pediatric life support during an emergency involving a young child. These evolving duties help reduce unnecessary ER visits and improve long-term outcomes. EMS providers often serve as the only consistent care contact for vulnerable individuals. This makes their ability to educate, refer, and support absolutely essential.
Changing Public Expectations and Burnout Pressures
Communities expect faster responses and broader support, yet staffing shortages challenge service delivery. Citizens often misunderstand what EMS teams can realistically provide. When expectations exceed available resources, tension rises on-scene and within agencies. Providers describe emotional exhaustion from constant exposure to trauma without proper recovery time. Without systemic support and recognition, burnout becomes a dangerous threat to workforce stability.
Inside the Ambulance: Stories from the Streets
“No Two Shifts Are Alike” — Urban Paramedic Realities
Gabriel Keller, a graduate of intensive paramedic training, now serves Hennepin EMS, regularly fielding overdose cases, shootings, and social crises. On any shift, one call might involve an elderly fall while the next is a high-speed crash. Crews often don’t get time to decompress between traumatic events. Their adaptability and sharp instincts define their effectiveness in these ever-changing environments.
How EMS Dispatchers Experience Emergencies From Afar
Dispatchers like Jamey Clark in Fort Worth manage life-and-death moments with only a voice on the line. In one call, she calmly guided a grandmother through delivering a baby alone at home. In another, she realized a caller’s wife had been stabbed by their own son. Her decisions shape patient survival before responders even arrive. This unseen side of EMS demands both emotional composure and lightning-fast clarity.
Split-Second Decisions That Stay With You
Field responders constantly make choices that carry long-term consequences, especially during high-stakes cardiovascular life support calls requiring fast, evidence-based decisions. These decisions require instinct, training, and courage in equal measure. Many EMS professionals revisit these moments mentally long after the shift ends. Though their role is high-pressure, they embrace the chance to make a difference when it matters most.
The Community Paramedic: Beyond Emergency Response
From Reactive to Proactive: Home Visits and Chronic Care
Don Thornton in Williamson County embodies the growing field of community paramedicine. Rather than reacting to crises, he checks in with patients to prevent future emergencies. He visits elderly patients with COPD, ensuring medication use and home safety. These efforts reduce repeat 911 calls and improve patient stability. This proactive approach turns EMS into an ongoing care solution.
Building Trust in Underserved Neighborhoods
Many community paramedics work in areas where people distrust healthcare systems. EMS professionals build relationships through consistent, non-judgmental care. They become trusted figures who deliver both medical aid and emotional support. By showing up regularly and offering practical help, they shift community perceptions. This trust transforms outcomes and fosters preventive care acceptance.
Why Preventative EMS is Reshaping the System
Preventative EMS helps reduce strain on overburdened emergency departments. Patients receive care earlier, often avoiding dangerous complications. This model saves costs while enhancing quality of life for chronically ill individuals. It also allows EMS professionals to apply their skills in new, deeply rewarding ways. Their evolving mission supports healthier communities through long-term connection.
Living the Job: The Long-Term Physical and Mental Toll
When Saving Lives Comes at a Personal Cost
Mike Doss, a retired Nashville paramedic, recalls how adrenaline masked the toll of 24-hour shifts. Years of skipped meals, poor sleep, and nonstop crises led to coronary artery disease. He regrets ignoring his own health while caring for others. EMS professionals often postpone self-care due to their demanding schedules. This lifestyle creates long-term risks without proper support systems.
PTSD, Sleep Deprivation, and the Invisible Injuries
Repeated exposure to trauma leaves invisible wounds. EMS workers report nightmares, hypervigilance, and emotional withdrawal as common signs. Lack of sleep only compounds these mental health challenges. Providers often hesitate to seek help, fearing stigma or judgment. Agencies that prioritize mental health access see greater retention and improved team morale. These findings align with a systematic review from the AHRQ, which found elevated rates of PTSD, depression, and suicide ideation among EMS professionals.
Retired Medics Reflect on What They’d Do Differently
Veterans of the field frequently urge younger crews to prioritize health early. They emphasize hydration, nutrition, and taking breaks during long shifts. Some also advocate for therapy as a tool for long-term emotional survival. Looking back, many wish they had advocated more for themselves. Their reflections highlight the need for cultural change within EMS environments.
When the Rescuer Becomes the Patient
EMS Professionals on Facing Their Own Medical Crises
Jason Bazelow, a critical care flight paramedic, suddenly became the patient when his aorta ruptured. The emergency unfolded quickly, and his survival depended on the same system he once served. Experiencing both sides of care changed how he views compassion and urgency. His story reminds providers that health risks don’t spare first responders. Being prepared for the unexpected becomes crucial, even for the prepared.
How Personal Health Emergencies Shift Their Perspective
After surviving major health events, EMS workers often adjust their approach to care. They gain new empathy for patients’ fear and uncertainty. Many say they now spend more time listening and reassuring. Personal experiences create more emotionally intelligent providers. These shifts benefit both patient care and team dynamics.
Lessons Learned from Being on the Other Side of the Stretcher
Survivors of medical emergencies often stress the importance of slowing down. Jason, for example, urges providers to check on their own health markers regularly. Many now advocate for more thorough wellness checks within EMS teams. Having lived through the system’s strengths and gaps, they become advocates for reform. Their insights offer practical wisdom to the next generation.
EMS and Mental Health Crises in 2025
Responding Without Resources: The Role EMS Plays in Mental Health
In many regions, EMS fills the gap left by underfunded psychiatric services. EMTs like Simon Gretton often encounter repeat callers in emotional distress. They de-escalate, offer short-term aid, and navigate scarce treatment options. Many cases stem from homelessness, addiction, or trauma. Without access to proper care, patients rely on EMS for stability.
Emotional Weight of Repeated Psychiatric Calls
Responders feel the emotional strain of returning to the same patients without long-term solutions. It creates frustration and sadness among teams. They want to help, but systemic limitations restrict their impact. Over time, this moral injury wears on even the most seasoned providers. A University of Colorado study confirms high levels of PTSD and …
Calls That Shouldn’t Be 911 – But Are
Many behavioral health emergencies fall outside the traditional EMS scope. Still, they get dispatched as high-priority 911 calls. Without training or backup, responders face unpredictable, high-stakes scenarios. Some systems now integrate crisis response teams or social workers. Expanding these models could relieve pressure on EMS and improve care alignment.
Realities in Rural vs. Urban EMS Work
Staffing Gaps and Resource Imbalances
Rural EMS agencies often operate with skeleton crews and outdated equipment. One provider might cover an area the size of a county. In contrast, urban crews face volume overload and tighter response times. Both environments require unique adaptation strategies. Addressing inequity means tailoring support to each system’s challenges.
Unique Challenges Faced by Small-Town EMTs
Rural EMTs often know their patients personally, which can complicate emotional boundaries. Limited hospital access forces longer transports and independent decision-making. With fewer backup options, errors carry greater risk. These providers display remarkable versatility and community dedication. Their experiences offer critical insights into decentralized emergency care.
What Urban EMS Can Learn from Rural Teams (and Vice Versa)
Urban teams could benefit from rural-style flexibility and deeper community integration. Rural agencies may adopt urban innovations like data tracking and cross-agency coordination. Exchange programs or ride-alongs can foster mutual learning. Each environment excels in different domains of problem-solving. Sharing insights builds a stronger, more resilient EMS workforce.
Voices from the Field: What Keeps Them Going
Stories of Survival, Gratitude, and Human Connection
EMS professionals often recall specific patients whose survival made the job worth it. One medic shared a thank-you letter from a boy whose life he saved. These moments validate the hard days and sleepless nights. Connection with patients builds lasting motivation. Recognition fuels continued service in a difficult career.
Why Some Medics Still Call It the Best Job in the World
Despite its hardships, many EMS workers express deep pride in their role. They appreciate the adrenaline, the trust, and the opportunity to serve. The unpredictability challenges them to grow constantly. For those drawn to service, EMS offers unmatched purpose. It remains a calling, not just a job.
The Power of Peer Support and Shared Experience
Talking with colleagues who understand the stress of the field provides critical relief. Informal debriefs after intense calls often become therapeutic rituals. Many agencies now encourage peer-led support programs. These efforts reduce stigma and build team cohesion. Shared experience creates strong professional bonds that buffer against burnout.
Frequently Asked Questions
What is the most challenging part of being an EMS provider in 2025?
Balancing growing responsibilities with limited resources is the top challenge. EMS professionals face rising patient needs without matching system support.
How has the EMS profession changed in the last five years?
The role has expanded from emergency-only care to include prevention, mental health, and community-based interventions.
What kind of training do community paramedics receive?
They undergo specialized education in chronic disease, patient counseling, and preventive care in addition to traditional EMT certification.
How do EMS workers manage emotional stress and trauma?
Many rely on peer support, therapy, and structured debriefing. Agencies are investing more in mental health programs and wellness resources.
3 Practical Tips for Aspiring or Current EMS Professionals
Build Resilience Through Structured Recovery Time
Schedule breaks and time off with intention, not guilt. Prioritize recovery as essential to longevity in the field.
Maintain Health Like Your Life Depends on It — Because It Might
Monitor blood pressure, hydrate regularly, and eat real meals even during chaotic shifts. Your future self will thank you.
Document and Debrief — Don’t Carry the Call Alone
Take time to write thorough reports and talk through difficult scenes. Both practices protect mental and legal wellbeing.
Honoring the Stories That Rarely Get Told
Why Listening to EMS Voices Matters Now More Than Ever
Public awareness often overlooks the humanity behind flashing lights. Real stories build empathy and drive better policy decisions. Listening helps shift public attitudes and deepen respect.
The Value of Preserving Real Accounts for Future Generations
Firsthand EMS experiences should be archived and shared. These stories guide new recruits and influence system improvements. They document the unseen reality of emergency care.
What Civilians Can Learn from the Professionals Behind the Sirens
Citizens gain a deeper appreciation for the resilience required in EMS roles. Understanding these pressures can change how we treat responders. Even small gestures of respect can go a long way.

Jeromy VanderMeulen is a seasoned fire service leader with over two decades of experience in emergency response, training, and public safety management. He currently serves as Battalion Chief at the Lehigh Acres Fire Control & Rescue District and is CEO of the Ricky Rescue Training Academy, a premier provider of online and blended EMT and firefighter certification programs in Florida.
Jeromy holds multiple degrees from Edison State College and the Community College of the Air Force, and is pursuing his MBA at Barry University. He maintains top-tier certifications, including Fire Officer IV, Fire Instructor III, and Fire Inspector II, and has served as a subject matter expert for a court case. He is a member or the Florida Fire Chiefs Association.
Jeromy also contributes to state-level fire safety regulation and serves on several hiring and promotional boards.

