Scope & Who This Is For
This page gives BLS learners and renewing providers a practical, field-tested playbook. You will find stepwise placement guidance, real-world workarounds, and short drills that actually stick. The focus stays strictly within BLS scope while still addressing common edge cases. Crews can use this during station training, mock codes, and skills refreshers. Supervisors can lift sections into quick huddles before shifts. The goal is simple: fewer pauses, cleaner shocks, and smoother teamwork when seconds matter.
Why Placement & Contact Quality Matter
Pads create a path for current that must cross critical myocardium. Good landmarks shape that path, while firm adhesion lowers impedance and preserves energy. Trapped air, moisture, and dense hair break contact and waste precious time. Those small problems turn into longer pauses, weaker shocks, and shaky team confidence. Teams that choreograph placement steps protect compression fraction and outcomes. Crews that practice micro-fixes get shocks delivered sooner and cleaner. Every decision here serves the same purpose: fast analysis and immediate compressions after each prompt.
Adult Pad Placement: Core Landmarks
Standard anterolateral placement (most adults)
Expose the chest completely and dry the target zones before anything else. Place the right pad just below the clavicle, slightly right of the sternum. Place the left pad on the left lateral chest along the mid-axillary line. Smooth each pad from the center outward to push out air and secure edges. Route the cable so it never drags across the airway or the compressor’s arms. Confirm edges lie flat with no wrinkles or gel ridges. Signal the AED tech that “pads are sealed,” then stay on compressions until analysis.
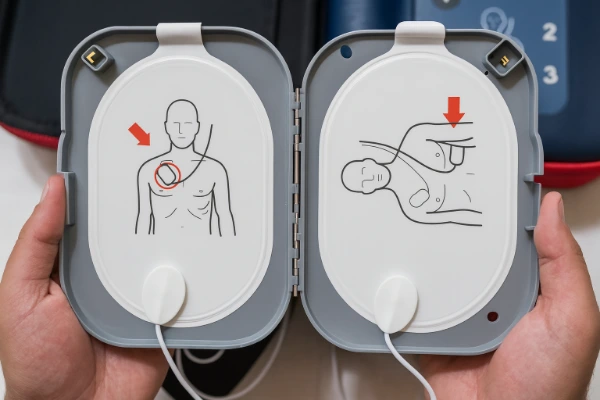
Alternative positions when needed
Front-back placement helps when a narrow chest risks pad overlap. Set the front pad centered on the sternum; place the back pad between the scapulae. Maintain clear separation so gel edges never touch across soft curves. Keep cable slack available to avoid edge lift during movement. Use the alternative layout only when anterolateral cannot maintain safe spacing. Move quickly, narrate your steps, and return to compressions immediately. Clean choreography here prevents long, silent pauses that erode perfusion.
Common errors to prevent
Pads over clothing, jewelry, or ECG leads cause false errors and poor contact. Wrinkles, air pockets, and dried gel defeat the purpose of expensive pads. Cables stretched tight lift corners during transfers and stair carries. Overlapping pads change the current path and weaken defibrillation. Taping down a bad pad wastes time when a quick replacement works better. Stacking new gel over old gel creates insulation, not adhesion. Fix only what affects signal quality, then drive the cycle forward.
Working Around Real-World Obstacles
| Scenario | Recommended Pad Layout | Fast Fix (≤30 sec) | Avoid / Watch Out | Team Cue | Notes |
|---|---|---|---|---|---|
| Pacemaker/ICD near clavicle | Anterolateral with 1" offset from device pocket | Identify pocket bulge, shift nearest pad ~1 inch, smooth edges | Pressing on pocket; cable tension that lifts corners | “Offset set—analyze next.” | Preserve vector; keep compressions moving |
| Medication patch under pad site | Anterolateral or Front-Back as chest size dictates | Glove, remove patch, wipe residue, dry skin, apply pad | Arcing risk over residue; long searches for ideal wipes | “Patch off—skin dry.” | Save patch for hospital handoff |
| Heavy chest hair blocking adhesion | Anterolateral preferred when separation maintained | Razor quick-swipes at pad footprints or “wax” with sacrificial pad; replace | Shaving entire chest; stacking new pad over old gel | “Pads sealed—analyze.” | Keep compressions going during prep |
| Wet/sweaty/rain-exposed chest or connectors | Anterolateral or Front-Back; choose best seal | Towel dry zones, fan 1 sec, reseat pads; dry connectors | Device exposed to rain; bagging during analysis | “Hands off—analyzing.” | Shield device; resume compressions immediately |
| Jewelry, piercings, ECG leads near pad edge | Maintain chosen vector; shift pad slightly if needed | Reroute leads; position pad away from metal without big detours | Time lost removing distant jewelry; cables pulling corners | “Contact confirmed.” | Seal and separation matter most |
| Bulky dressings or chest wounds | Anterolateral or Front-Back on intact skin zones | Replace only blocking dressing; pick intact skin and seal fully | Placing over open wounds; large layout changes mid-code | “Seal good—continue.” | Announce changes to sync analysis timing |
| Small pediatric chest; pads risk touching | Front-Back layout; pediatric pads or attenuator when available | Center front pad on sternum; back pad between scapulae; check edges | Delay searching accessories; pad overlap across sternum | “Front-back set.” | Use adult pads if pediatric unavailable—do not delay |
| AED won’t analyze; motion or artifact | Any layout with firm, full-edge seal | Call “hands off,” pause bagging, smooth pads, reseat connectors | Repeated button presses; analyzing while movement continues | “Chest quiet—analyze.” | Swap pads/device if issue persists |
| No pediatric pads/attenuator available | Use adult pads; prefer Front-Back for separation | Ensure pads don’t touch; proceed without delay; document supply gap | Skipping analysis while searching supplies | “Adult pads used.” | Report to logistics after call |
| Transport moves; pad edges lifting | Keep chosen layout; re-seal edges after lifts | Dry sweat, smooth corners, replace problem pad promptly | Babysitting bad pad with tape while cadence slips | “Edges good—continue.” | Quick fix then back to compressions |
| Low battery or damaged cable mid-code | Any layout; keep seal while swapping gear fast | Swap battery/device; grab backup; maintain compressions during change | Pausing compressions for gear searches or debates | “Backup in—continue.” | Log failure; fix readiness post-event |
Implanted pacemakers/ICDs
Identify a generator pocket by the small, firm bulge under skin near the clavicle. Offset the nearest pad at least an inch while keeping the same vector. Smooth the pad without pressing directly on the device pocket. Narrate the offset so the AED tech anticipates the cable route. Keep compressions moving while you adjust position quickly. Recheck edges once after the first analysis to confirm contact. Note the device during debrief so training covers the scenario again.
Transdermal medication patches
Glove up and remove any patch under a planned pad immediately. Wipe away residue and dry the skin because leftover gel compromises adhesion. Apply the pad only after the skin feels dry and clean to touch. Save the patch for hospital handoff and documentation. Keep the compressor on rhythm while the AED tech works the chest. Avoid hunting for perfect wipes when towels will do the job. Clear, short commands keep the sequence predictable and fast.
Heavy chest hair
Target the footprint only and make two quick razor swipes per site. If no razor exists, press a sacrificial pad, rip it off, then place a fresh pad. Avoid shaving the whole chest, which costs time and adds mess. Smooth edges carefully because short stubble can still lift corners. Keep the compressor working while the airway provider prepares ventilations. Recheck adhesion after any large movement onto a stretcher. Replace any pad that repeatedly lifts despite smoothing.
Wet, sweaty, or rainy environments
Dry the placement zones with a towel and give a quick fan for a second. Apply pads and press outward until edges seal firmly all around. Dry connectors if rain or sweat touched them during extrication. Shield the device itself to prevent error prompts or screen failures. Quiet the chest for analysis by pausing bagging and calling “hands off.” Resume compressions the instant the device finishes speaking. That rhythm keeps the team calm even when weather isn’t.
Jewelry, piercings, monitoring leads
Shift pads slightly to avoid direct contact with metal without losing the vector. Reroute ECG leads so they never slide under pad edges or tug corners. Do not waste time removing distant jewelry that doesn’t affect adhesion. Focus on seal, separation, and a clean current path every time. Confirm the device reads a stable signal before pressing analyze. Maintain cable slack so nothing pulls during switches or lifts. Then move the cycle forward without debate.
Dressings, trauma, and skin integrity
Work around bulky dressings while protecting a full, flat seal. Replace only the dressing that blocks proper pad contact. Choose intact skin that holds gel without slipping across moisture. Avoid placing pads directly over open wounds when alternatives exist. Keep your anterolateral or front-back vector consistent despite obstacles. Announce changes so the whole team predicts analysis timing. Small, clear statements preserve momentum and reduce dead space.
Pediatric AED Use (Infants & Children)
When to use pediatric pads/attenuators
Read the pad package for age or weight guidance as you open it. Use pediatric pads or attenuators when the device clearly recommends them. Default to adult pads if appropriate pediatric options are unavailable. Never delay analysis while hunting for ideal accessories during a code. Confirm full-edge adhesion before analysis and after any movement. Keep the team on the standard two-minute cadence. Debrief supply gaps so logistics fixes the problem, not the next crew.
Placement options to avoid pad overlap
Use anterolateral when pads fit with clean separation on the chest. Switch to front-back for small torsos where edges might touch. Check visually that gel borders never meet across the sternum or axilla. Smooth both pads and confirm a firm seal along the entire perimeter. Keep cable slack clear of little arms and straps. Recheck adhesion after transfers and car-seat extrications. Simple checks here prevent frustrating “poor contact” loops.
Frequent pediatric errors
Pad overlap remains the top error on infants and toddlers. Long accessory searches burn minutes while perfusion falls. Motion during analysis blocks rhythm detection and delays the next step. Tiny air pockets at edges fool devices more than crews expect. Tape rarely fixes a lifting pad as well as a replacement does. Coach ventilations because over-bagging steals time and causes artifact. A confident script prevents drift when nerves spike.
Pregnancy: Safe, Effective BLS Defibrillation
What changes for BLS CPR
Use standard hand placement and compression depth because effective compressions matter most. Assign one rescuer to perform manual left uterine displacement continuously. Lateral displacement reduces aortocaval compression and improves venous return. Rotate compressors on schedule so fatigue never softens depth or recoil. Script analysis windows to keep pauses short and predictable. Coach ventilations to avoid hyperinflation during critical moments. That shared cadence keeps care steady while emotions run high.
Defibrillation points specific to pregnancy
Place pads in standard positions unless separation fails on a narrow chest. Deliver shocks without delay because maternal survival drives fetal survival. Keep oxygen delivery away from pad edges and potential spark zones. Announce “clear” loudly and look before discharging every shock. Resume compressions immediately when the device finishes speaking. Reassess displacement after position changes or transport bumps. Then document pregnancy-specific actions during debrief for learning continuity.
Device Behavior: “Analyze,” “No Shock Advised,” and Errors
When the AED won’t analyze
Control motion first with a crisp “hands off” and a brief ventilation pause. Smooth pads again if the device reports poor contact or artifact. Check connectors for a loose fit or unexpected moisture. Clear blankets, straps, or clothing that press against pad edges. Retry analysis after fixing the most likely cause quickly. If prompts persist, swap pads or the device before tempo collapses. Keep compressions on schedule while the tech troubleshoots.
“No shock advised” in an arrest scenario
Return to compressions immediately when the device advises no shock. Do not chase shocks when the rhythm remains non-shockable. Hold the two-minute cycle and prepare the next analysis window. Reseat pad edges and verify cable routing during compressions. Coach compressor depth, rate, and recoil as a constant loop. Keep the airway simple and the ventilation cadence steady. That discipline buys the next chance for a meaningful rhythm change.
Battery, cartridge, and cable issues
Watch status lights and battery meters during daily checks and after dispatch. Swap batteries at the first true low indicator; don’t gamble mid-code. Replace damaged cables and keep a spare in the same pouch. Stage a backup device where crews can grab it blindfolded. Train the backup grab so nobody asks questions under stress. Log failures promptly so maintenance closes the loop. Readiness lives in small habits, not lucky breaks.
Team Choreography That Protects Compression Fraction
Four essential roles on a BLS team
Assign compressor, ventilator, AED tech, and timekeeper in the first breaths. Give the compressor permission to ignore screens and focus on mechanics. Ask the ventilator to protect cadence and avoid over-ventilation. Put pads, cables, and prompts under the AED tech’s control. Let the timekeeper own switches and announce analysis windows out loud. Use the same script across crews to avoid confusion. Shared language turns chaos into a familiar rhythm.
Clean analysis windows with minimal pause
Say the same words before every analysis to quiet the chest. “Stop compressions, stop bagging, hands off” sets the stage cleanly. Press analyze only after visual confirmation of stillness. Keep eyes on the patient, not the screen animations. Resume compressions the instant the device finishes speaking. Pre-charge or prepare as your protocol allows without stalling. Consistency shortens pauses more than heroics ever will.
Switches and cable management
Switch compressors every two minutes or sooner if form slips. Count down the final ten seconds so hands move on cue. Step the incoming rescuer into position while the outgoing steps back. Route cables outside knees and away from the airway to prevent snags. Keep slack so corners don’t lift during vigorous compressions. Recheck edges after each switch and any lift to a stretcher. That tiny ritual keeps analysis clean later.
Safety Checks Everyone Owns
Shock safety
Scan the scene and confirm nobody touches the patient before discharging. Keep oxygen away from pad edges to reduce ignition risk. Say “clear” loudly, look left and right, then press shock. Check your own hands, clothing, and cables during the sweep. Expect feet, knees, and elbows to creep toward the patient under stress. Practice the sweep so it happens even when noise explodes. Then resume compressions without waiting for coaching.
Adhesion rechecks after movement
Movement loosens edges more often than crews realize. Smooth corners after stair chairs, lifts, and stretcher bumps. Replace a problem pad rather than babysitting it with tape. Dry sweat as needed because moisture sneaks under edges fast. Announce re-adhesion so the team expects brief handling. Fix only what affects signal quality to protect cadence. Then drive back to compressions with purpose.
Micro-Drills to Build Automaticity
30-second pad placement sprint
Run a timed expose-dry-place-smooth sequence with a visible clock. Rotate roles and keep obstacles changing each round. Track times on a whiteboard near the device compartment. Celebrate progress and cut times with tiny, repeatable tweaks. Shoot for realism by adding shirts, sweat, and mild rain simulation. Pair each sprint with a quick analysis rehearsal. Repetition beats longer, infrequent mega-drills.
Wet-skin and sweat simulation
Mist the chest with a spray bottle and start the clock. Towel briskly, fan once, and seal both pads completely. Recheck edges after a mock lift or transfer. Note moisture thresholds that trigger device complaints. Teach crews to fix only the step that matters. Keep compressions rolling while the AED tech works the chest. Repeat until the workflow feels boring and automatic.
Pacemaker/ICD offset practice
Mark a fake pocket with a small piece of tape. Offset the nearest pad one inch while preserving the vector. Smooth edges firmly and confirm a clean perimeter. Practice cable routes that avoid the altered pad position. Debrief the feel and the look so recognition speeds future cases. Repeat until nobody needs verbal guidance. That’s when the habit is real.
Pediatric front–back reps
Use a pediatric manikin or marked torso and run quick reps. Choose front–back when anterolateral risks edge contact. Confirm full separation visually and by feel along the edges. Keep cable slack away from small arms and straps. Recheck after moves because tiny chests shift pads easily. Track reps like sprints to build confidence. Speed follows certainty in layout choice.
Motion-free analysis rehearsal
Practice the three-line script that freezes motion on demand. Coach ventilations to quiet hands during the analysis window. Watch for wandering fingers, coats, or straps across the chest. Resume compressions the instant the device finishes speaking. Record pause length and aim for steady reductions. Repeat until the script runs without conscious effort. That’s how cadence survives chaos.
Stocking & Daily Readiness
What must be in the kit
Carry spare adult pads, pediatric pads or attenuators, and razors. Keep towels, wipes, gloves, and a backup battery in the same pouch. Add a spare cable or a full backup device when resources allow. Place a one-page drill card beside the AED for quick refreshers. Include a simple debrief sheet with time fields and checkboxes. Standardize layout across units so muscle memory transfers. Small logistics decisions decide big moments.
Daily quick check
Open the device and verify the status light and battery meter. Inspect pad packaging for expiration and seal integrity. Run fingers along cables to feel for kinks or frays. Confirm pediatric accessories exist or document an alternative plan. Check that towels and razors sit exactly where hands expect them. Close with a brief verbal checklist between partners. Sign the log so accountability lives in black and white.
Post-event reset
Replace used pads and batteries as soon as the call ends. Wipe connectors dry and stow the device in a protected spot. Restock towels, wipes, and razors before you clear the bay. Update the log with supply numbers and any gear issues. Flag broken items for repair rather than hiding them back in the bag. Share one quick win and one focus item during cleanup. Readiness returns before the next tone drops.
Documentation & Debrief Prompts
What to capture
Record time to pad placement and time to first analysis. Note obstacles like hair, moisture, or implanted devices. Capture compression fraction highlights and major pause reasons. Document supply gaps that changed layout or delayed analysis. Write one improvement you will drill during the next shift. Share one success that other crews can copy easily. Close the note so learning turns into action.
One win / one focus
Pick one habit worth celebrating because progress fuels morale. Choose one specific improvement and convert it into a drill. Keep goals measurable, time-bound, and easy to repeat. Schedule the drill before the next shift change. Post a reminder near the device so nobody forgets. Resurface the goal at the start of the next huddle. That rhythm turns ideas into consistent performance.
Practical Wrap-Up: Make This Muscle Memory
Turn these steps into short, frequent practice so they survive stress. Bring edge cases and placement questions to our AHA BLS for Healthcare Providers course and sharpen them with instructors who run real cases. If you need enrollment details or scheduling windows, visit the Application Process page and plan your next session. Keep a drill card by the device and track your times for a month. Share best practices across shifts so the whole team benefits. The first clean analysis, the first fast shock, and the first strong restart all start here.
