Key Takeaways
- Stock pediatric-sized equipment, verify updated dosing protocols, and run high-fidelity drills with regular BLS / PALS renewals before classes resume.
- Use PAT, JumpSTART, and age-specific vital sign norms to triage quickly, identify silent chest, and avoid unnecessary spinal immobilization.
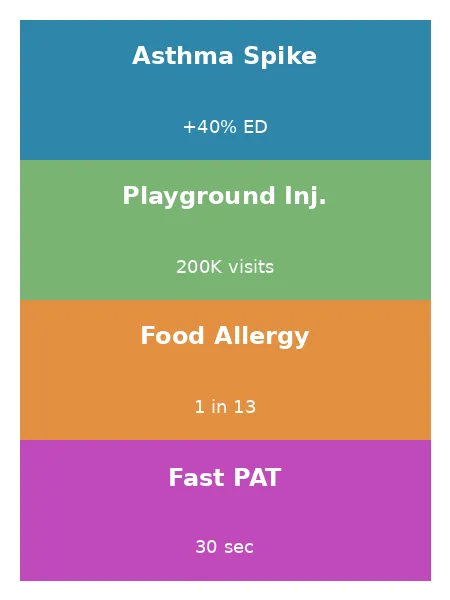
- Integrate student health action plans, nurse insights, and community surveillance to anticipate the September asthma spike and rising school-year allergy calls.
Early-School-Year Risk Landscape
The September Asthma Spike: Epidemiology and Triggers
Schools reopen after summer break, and respiratory viruses surge among children. The rise sparks a predictable wave of pediatric school emergencies centered on asthma. Viral infections combine with allergens lingering in cleaned buildings, triggering bronchospasm within days of the first bell. An NIH study found pediatric asthma admissions climb nearly forty percent during this two-week window. EMS agencies prepared with extra albuterol kits manage calls efficiently and protect hospital capacity. Early stocking and staff refresher sessions should happen in July to stay ahead.
Playground Trauma Trends in the First Eight Weeks
During recess, lively games bring enthusiasm and elevated injury risks. The U.S. Consumer Product Safety Commission counts more than two hundred thousand emergency visits yearly for playground injuries. Playground structures endure heavy summer heat that loosens bolts and cracks surfaces. Falls from swings or climbing walls produce upper-extremity fractures at twice the rate of leg breaks. Concussions also rise because younger children struggle with depth perception on new equipment. Crews need pediatric splints, analgesia protocols, and neuro checklists ready before the first bell rings. Early inspections by school maintenance teams complement EMS preparedness and reduce incident frequency.
Rising Food and Environmental Allergies in School Settings
Cafeterias introduce new menus that expose students to unfamiliar food proteins. Roughly one in thirteen children lives with a diagnosed food allergy. Classroom experiments, art supplies, and field trips add pollen, latex, or insect venom threats. First-time reactions often occur in September when vigilance still develops among teachers and peers. Epinephrine delivered within minutes halts progression and prevents fatal outcomes every school year. Agencies must verify each unit carries weight-based auto-injectors and updated anaphylaxis protocols. Collaboration with nutrition staff improves label clarity and minimizes accidental exposures.
Pre-Arrival Intelligence: Leveraging School Health Data
Integrating Individual Health Action Plans into ePCR Systems
Electronic patient care records become more valuable when they store student-specific action plans. Uploaded documents list triggers, preferred medicines, and emergency contacts, allowing crews to prepare en route. Quick access eliminates backpack searches and compresses on-scene timelines significantly. Implementation requires summer coordination among IT teams, nurses, and privacy officers. Agencies that finish integrations before orientation week see faster medication delivery and fewer complications. Annual audits confirm information accuracy and strengthen trust between schools and responders.
Building Relationships with School Nurses and Coaches
School nurses track daily health issues and share vital insights with EMS partners. Quarterly meetings create channels for discussing incident statistics and equipment needs. Athletic coaches highlight practice schedules that often coincide with dehydration or injury peaks. Joint tabletop exercises cultivate familiarity and streamline communication during real crises. Parents appreciate unified messaging when professionals demonstrate coordinated preparation before emergencies strike. These relationships reduce response delays and improve patient outcomes throughout the academic year.
Using Community Surveillance for Seasonal Alerts
Local public-health dashboards highlight spikes in infections or pollution that precede call surges. Dispatch centers can subscribe to automated alerts and adjust staffing hours accordingly. Schools contribute absentee data that often signals looming respiratory outbreaks. Agencies viewing these trends shift additional units toward affected zones proactively. Data-driven readiness maintains response times even when volume rises sharply. Sharing surveillance findings with educators fosters a culture of prevention.
Rapid Pediatric Assessment Frameworks
Pediatric Assessment Triangle (PAT): Visual Clues in 30 Seconds
Rapid scene sizing begins with the Pediatric Assessment Triangle, completed before hands contact the child. Crews observe appearance, effort of breathing, and skin circulation from several feet away. Loud crying typically indicates patent airway and good perfusion, whereas silence may signal impending collapse. The entire assessment consumes fewer than thirty seconds yet guides priority decisions. Immediate identification of respiratory failure allows faster medication delivery on scene. Ongoing reassessments every two minutes verify treatment effectiveness for safety.
JumpSTART Triage for Mass-Casualty Playground Events
Multiple-victim playground incidents demand triage that respects children’s unique physiology. JumpSTART evaluates respiration, consciousness, and perfusion while accounting for immature airway reflexes. Responders give five rescue breaths to apneic children with pulses before categorizing. This step prevents premature black tagging of salvageable patients entirely. Clear color-coded tags reduce confusion among mutual-aid crews during stress. Training on the algorithm during drills ensures confident execution when chaos emerges.
Age-Specific Vital Sign Norms and Red-Flag Thresholds
Heart rate, respiratory rate, and blood pressure shift quickly across pediatric age brackets. A newborn may reach 160 beats per minute, whereas a teenager rests nearer 90. Accurate interpretation prevents mislabeling compensated shock as normal in reports. Color-coded reference tools attached inside monitor cases speed decision-making during care. Mobile apps that auto-calculate red flags further reduce cognitive load. Crews should update these resources annually to match evolving guidelines.
| Age Group | Heart Rate (normal bpm) |
Respiratory Rate (normal / min) |
Red-Flag Heart Rate (> bpm) |
Low Systolic BP (≤ mmHg) |
|---|---|---|---|---|
| Infant (0–12 mo) | 100 – 160 | 30 – 53 | 180 | 70 |
| Toddler (1–3 yr) | 90 – 150 | 24 – 40 | 170 | ≤ 70 + (2 × age) |
| Preschool (3–5 yr) | 80 – 140 | 22 – 34 | 160 | ≤ 70 + (2 × age) |
| School-age (6–12 yr) | 70 – 120 | 18 – 30 | 150 | ≤ 70 + (2 × age) |
| Adolescent (13–18 yr) | 60 – 100 | 12 – 20 | 130 | 90 |
Airway and Respiratory Management for Pediatric Asthma Exacerbations
Evidence-Based Pharmacology: Nebulizers vs. MDIs in the Field
Selecting between nebulizers and metered-dose inhalers depends on distress severity and oxygen availability. Spacers paired with inhalers deliver similar bronchodilation while conserving precious tank volume. Nebulizers remain valuable when severe fatigue impairs coordinated inhalation ability. Stocking both tools ensures appropriate therapy regardless of scenario everywhere. Staff training should emphasize quick device assembly to minimize hypoxic intervals. Recording response times supports quality improvement initiatives across departments annually.
Oxygen Delivery Modalities and Monitoring
Hypoxia worsens fatigue and anxiety, so immediate oxygen supplementation remains critical. Cannulas supply sufficient oxygen for mild distress while preserving patient comfort. Non-rebreather masks achieve higher concentrations when saturation drops below ninety-four percent. Continuous pulse oximetry guides timely escalation or tapering of flow. Avoiding hyperoxia prevents oxidative injury and aligns with modern guidelines. Tracking saturation trends helps evaluate treatment effectiveness during transport periods.
Avoiding Common Pitfalls (Silent Chest Recognition, Over-Ventilation)
A silent chest signals dwindling airflow requiring urgent bronchodilator escalation. Providers must auscultate both axillae after every treatment round carefully. Over-ventilation during bagging can trap air and worsen hyperinflation quickly. Deliver slow, gentle breaths synchronized with visible chest rise always. End-tidal carbon dioxide monitoring confirms adequate ventilation without inducing barotrauma. Team debriefs after calls reinforce best practices and identify areas needing review.
Musculoskeletal and Head Injuries from Playground Incidents
Scene Safety and Mechanism-of-Injury Evaluation
Arriving crews scan the playground for hanging chains, damaged surfaces, and panicked bystanders. Witnesses describe fall heights, impact points, and force directions clearly. This information directs attention toward possible head, spine, or abdominal injuries. Teams designate a safety officer to manage crowd control and equipment hazards. Clear roles allow medics to focus on patient stabilization tasks. Early hazard mitigation also protects responders from secondary accidents onsite.
Focused Neuro and C-Spine Decision Algorithms
Selective spinal-precaution algorithms reduce unnecessary immobilization without sacrificing safety today. NEXUS-PEDS examines midline tenderness, altered consciousness, and distracting injuries carefully. Absence of these findings supports gentle movement onto padded stretchers without collars. Glasgow Coma Scale modifications detect subtle pediatric neurological decline early. Every reassessment includes pupil checks and limb strength evaluation routine. Efficient yet thorough exams speed departure and lower on-scene time.
Pain Control, Splinting, and Transport Considerations
Early intranasal analgesia improves cooperation and simplifies splint placement greatly. Vacuum devices mold to small limbs and permit painless radiography later. Crews secure slings snugly but leave fingertips exposed for perfusion checks. Soft padding reduces vibration discomfort during ambulance acceleration and braking. Clear explanations keep children informed and less fearful throughout transport. Documenting pain scores before and after treatment supports quality assurance metrics.
Identifying and Treating Pediatric Anaphylaxis
Recognizing Biphasic Reactions and Hidden Allergens
Anaphylaxis can rebound hours after initial stabilization, challenging complacent caregivers. Hidden triggers often lurk in craft supplies, science experiments, or insect nests. Crews inspecting surroundings identify allergens and prevent secondary exposures quickly. Extended observation of thirty minutes or more detects emerging symptoms early. Families receive education on rebound timing and emergency plan updates. Strong communication supports adherence and reduces repeat calls significantly.
Epinephrine Dosing, Auto-Injectors, and Manual Syringes
Intramuscular epinephrine at 0.01 milligrams per kilogram remains the gold-standard intervention. Auto-injectors provide rapid delivery yet lack flexibility for infants below fifteen kilograms. Syringe administration demands accurate calculation and training drills bolster competence. Agencies must stock both methods and verify expiration dates monthly. Crews announce dose and route aloud to encourage double-checking immediately. Prompt administration saves lives and prevents cardiac collapse entirely often.
Post-Intervention Observation and Documentation Best Practices
Continuous monitoring, every five minutes, detects early relapse after epinephrine administration. Vitals including blood pressure, oxygen saturation, and mental status reveal subtle deterioration. Documentation records onset, dose, response, and time of transport clearly. Receiving hospitals appreciate concise yet comprehensive handoffs during arrivals always. Early notification encourages preparation of pediatric critical-care teams well. Thorough charts also protect crews during retrospective audits later periods.
Psychological First Aid for Children and Caregivers
Age-Appropriate Communication Techniques
Children respond better when responders kneel, maintain eye contact, and explain steps clearly. Using simple language avoids confusion and preserves dignity for everyone. Distraction techniques like phone cartoons or bubble blowers lower anxiety. Calm demeanors help regulate heart and respiratory rates quickly too. Parents witnessing kindness feel reassured about their child’s care quality. Such interactions build long-term community trust that strengthens support networks.
Managing Parental Presence to Lower Scene Anxiety
Bringing parents into the treatment process lowers anxiety for both child and caregiver. Assigning a liaison communicates updates without distracting primary medics ever. Parents can assist by holding masks or comforting blankets during interventions. This inclusion fosters cooperation and reduces scene conflict significantly today. Clear expectations also prevent unsafe interference during complex procedures always. Post-incident feedback sessions refine the approach continually across teams citywide.
Crew Mental Health After High-Stress Pediatric Calls
Pediatric calls carry high emotional weight that can erode crew resilience. Early defusing sessions allow expression of stress before it festers. Peer-support programs offer confidential counseling and resource referrals to everyone. Leaders must model healthy coping by attending sessions themselves publicly. Routine mental health training normalizes help-seeking behavior among professionals everywhere. Lower burnout translates into safer, more compassionate patient care always.
Equipment Readiness and Protocol Optimization
Stocking Pediatric-Sized Airway, Vascular, and Immobilization Tools
Adult equipment often fails on small airways or limbs, making size-appropriate tools essential. Every ambulance should carry neonatal through adolescent bag-valve masks readily. Length-based tapes guide quick selection of airway adjuncts and vascular catheters. Pediatric tourniquets control hemorrhage without crushing delicate tissue vessels below. Inventory checks each shift catch missing or expired items promptly. Senior crew chiefs maintain current ACLS certification to coordinate advanced airway and circulatory interventions when school staff initiate CPR. Consistent readiness saves critical seconds during high-stress calls for patients.
Updating Standing Orders for Epinephrine and Bronchodilators
Annual protocol reviews ensure current dosing standards reach the field swiftly. Mandatory BLS for healthcare providers refreshers every two years reinforce the CPR foundation every pediatric resuscitation depends on. Medical directors analyze new studies on epinephrine, bronchodilators, and steroid timing. Approved changes migrate into digital reference apps accessible offline immediately. Training sessions reinforce updates and answer crew questions in detail. Version control prevents outdated paper copies from circulating widely. Metrics then track adherence and patient outcomes closely yearly.
Training Drills: Simulation Scenarios for Back-to-School Hazards
High-fidelity simulations replicate common school-year emergencies and strengthen muscle memory. Scenarios include asthma arrests, anaphylaxis collapses, and multi-victim fall incidents. Real medications and functional monitors reproduce physiological changes on manikins. Graduates fresh from accredited paramedic training programs bring current dosing skills into every scenario. Video playback during debriefs enhances retention and highlights areas for refinement. Regular repetition converts practice into instinct that surfaces under pressure. Departments that pair high-fidelity drills with regular PALS renewal keep pediatric algorithms sharp for the September surge.
3 Practical Tips
Pre-Load School Health Plans into Tablets Before August
Uploading action plans before August prevents frantic searches during crisis moments. IT teams should establish cut-off dates and completion dashboards for clarity. Validation calls with nurses verify current medications and parent contacts. Crews appreciate reliable data when cellular service drops during storms. Early effort yields smoother operations all semester for every team. Continuous updates maintain accuracy as student populations shift through turnover.
Assign a Dedicated “Family Liaison” Role on Every Pediatric Call
A dedicated family liaison frees clinicians to focus on airway, breathing, and circulation. This role explains procedures, gathers history, and answers pressing questions. Relatives feel informed, reducing scene tension and enhancing cooperation significantly. Clear boundaries also protect sterile fields and equipment from contamination. After transport, the liaison provides contact information for follow-up care. Agencies should train volunteers or EMTs for this essential function.
Add a “September Spike” Quality-Assurance Flag to Monitor Asthma Intervals
Tagging August–September respiratory calls with a “school spike” label supports rapid auditing. Quality teams review flagged incidents weekly and identify delays or supply shortages. Immediate feedback guides protocol tweaks before trends worsen for patients. Transparent reporting motivates crews to maintain accurate documentation on scenes. Dashboard visualizations track improvements across districts in near real time. Data-driven insights justify funding for additional pediatric supplies and training.
Frequently Asked Questions
What is the first medication EMS should administer for suspected pediatric anaphylaxis?
Intramuscular epinephrine should be administered immediately at weight-based dosing everywhere. Deliver the shot in the anterolateral thigh without delay whatsoever.
How do I quickly differentiate between mild and severe asthma in a child on scene?
Observe work of breathing, speech ability, and chest sounds closely. Severe cases feature single-word speech, accessory muscle use, or silent chest.
When should C-spine immobilization be applied in playground falls?
Apply immobilization after high-energy mechanisms, loss of consciousness, or neurological deficits. Absence of these findings allows movement with careful support instead.
What documentation elements are legally critical after treating a school-related pediatric emergency?
Record timelines, assessments, interventions, and communications with caregivers on scene. Include medication doses, vital trends, and identified hazards for comprehensive review.
Key Takeaways for EMS Crews This School Year
Back-to-school season presents predictable hazards that EMS agencies manage through preparation and collaboration. Stock child-specific equipment, refine assessment frameworks, and update protocols before August arrives. Build partnerships with school staff and leverage community surveillance for early warnings. Support responder mental health to maintain high performance under stress. Consistent quality reviews transform lessons into safer outcomes for every student.
Jeromy VanderMeulen is a seasoned fire service leader with over two decades of experience in emergency response, training, and public safety management. He currently serves as Battalion Chief at the Lehigh Acres Fire Control & Rescue District and is CEO of the Ricky Rescue Training Academy, a premier provider of online and blended EMT and firefighter certification programs in Florida.
Jeromy holds multiple degrees from Edison State College and the Community College of the Air Force, and is pursuing his MBA at Barry University. He maintains top-tier certifications, including Fire Officer IV, Fire Instructor III, and Fire Inspector II, and has served as a subject matter expert for a court case. He is a member or the Florida Fire Chiefs Association.
Jeromy also contributes to state-level fire safety regulation and serves on several hiring and promotional boards.

