Key Takeaways
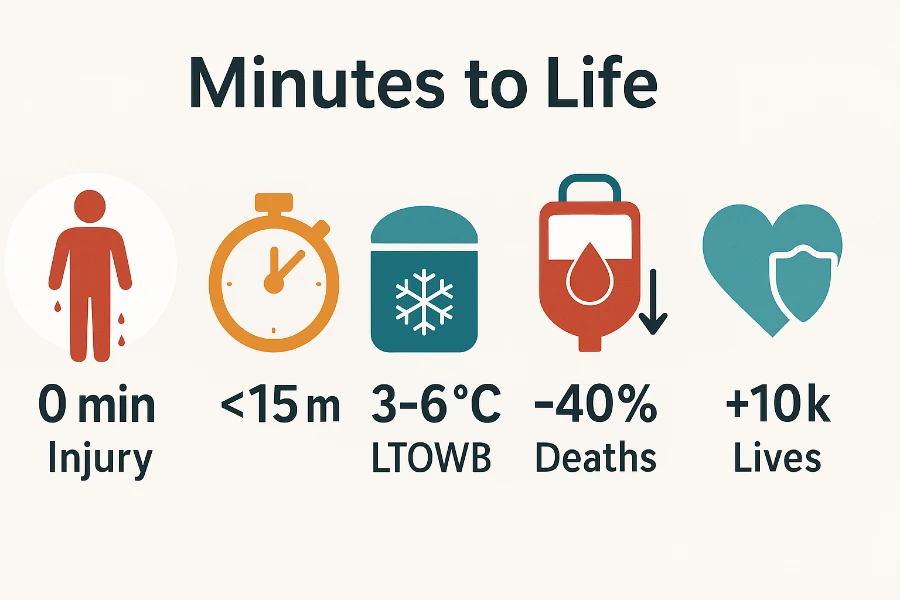
- Universal low-titer whole blood can cut preventable trauma deaths and boosts survival when infused inside 15 minutes.
- Validated coolers, rotation plans, and portable warmers keep blood viable, reduce wastage, and fit diverse EMS settings.
- Comprehensive training, data dashboards, and emerging reimbursement codes sustain programs and drive continuous improvement.
Why Whole Blood at the Point of Injury Matters
Trauma remains the nation’s leading preventable killer after age one. Low-titer O-positive whole blood cuts exsanguination deaths when crews infuse within fifteen minutes. Researchers at the American College of Surgeons estimate universal access could spare about ten-thousand American lives each year. Paramedics now carry validated coolers that safeguard clotting factors on the way to surgery. This article unpacks the science, logistics, training, and leadership steps that turn evidence into outcomes.
Historical Shift in Resuscitation Strategies
From Crystalloid Dominance to Balanced Component Therapy
For decades, EMS relied on crystalloids despite lessons emphasized during paramedic training about dilutional coagulopathy. Trauma surgeons then adopted balanced components to mimic whole-blood ratios of red cells, plasma, and platelets. Multiple bags slowed scenes and complicated compatibility checks on dark highways. Single-unit whole blood solved these pain points while improving clot strength and oxygen delivery. Agencies soon realized the older product offered a modern advantage.
Military Validation of LTOWB and the Civilian Knowledge Gap
Battlefield medics in Iraq and Afghanistan documented lower mortality using low-titer O-positive whole blood. Civilian trauma systems studied those results and launched helicopter pilots that echoed military success. Early adopters struggled with donor screening rules until regional coalitions standardized titers and paperwork. State regulators then issued waivers that paved the way for ground-unit rollouts. Momentum shifted from experimental to essential within five years.
Evidence Base for Prehospital Whole-Blood Use
Key Civilian and Military Studies on Mortality Reduction
A multicenter civilian study showed forty-percent fewer deaths when first units were whole blood. Military registries confirmed survival gains and recorded fewer transfusion reactions than component therapy. Texas air-medical crews reported sixty-seven-percent survival among severely injured recipients after program launch. Consistency across settings convinced policymakers that evidence had matured. Clinical focus moved from “if” to “how” agencies should deploy whole blood.
Professional Guidelines and Position Statements (ACS, NAEMSP, PHTBC)
The American College of Surgeons recommends low-titer whole blood whenever systems can uphold strict cold-chain standards. The National Association of EMS Physicians echoes that stance and details quality-assurance checkpoints. Prehospital Blood Transfusion Coalition guidelines outline donor titers, lot tracking, and training hours. Leadership teams leverage these documents to secure grants and hospital partnerships. Uniform standards also protect crews from medico-legal exposure.
Program Planning and Stakeholder Alignment
Medical Oversight, Legal Authority, and Protocol Drafting
Medical directors champion protocols, secure scope-of-practice approvals, and sign standing orders. Legal advisors clarify interstate transport rules and indemnity language. Clinical committees craft concise decision trees covering scene criteria, dosing, and reaction management. IT teams integrate lot numbers into electronic documentation for real-time audits. Early alignment speeds launch while guarding patient safety.
Partnering With Hospitals and Regional Blood Centers
EMS leaders negotiate with transfusion services for consistent low-titer supply and fourteen-day rotations. Blood centers handle donor screening, compatibility tests, and scheduled deliveries that match crew shifts. Hospitals accept unused units at rotation deadlines, reducing wastage and protecting budgets. Memorandums of understanding assign temperature-monitoring responsibilities and restocking triggers. Strong partnerships keep coolers full and bureaucratic hurdles low.
Blood Product Selection and Safety Parameters
Donor Screening and Low-Titer Thresholds
Blood centers label units “low-titer” when anti-A and anti-B levels stay below 1:256. Scheduled retesting ensures donors remain eligible and antibody profiles stable. Clear labeling and digital barcodes give crews instant compatibility confirmation. Single-product simplicity eliminates multibag confusion during chaotic scenes. Patients benefit from rapid, clot-friendly transfusions with minimal reaction risk.
Rh-Negative Considerations for Females of Child-Bearing Age
Programs carry contingency plans to protect future pregnancies from Rh sensitization. Some services stock limited O-negative whole blood for potential child-bearing patients. Others switch to component therapy when demographics demand. Decision trees help crews weigh fetal risk against lethal hemorrhage. Documentation flags choices for hospital follow-up and counseling.
Cold-Chain Logistics and Specialized Equipment
Cooler Validation, Temperature Monitoring, and Data Logging
Guidance from the Joint Trauma System shows phase-change coolers maintain three-to-six-degree ranges for over twenty-four hours. Bluetooth probes stream temperatures to cloud dashboards and alert supervisors to rare deviations. QR codes link each cooler to patient care reports, easing audits. Digital records shorten regulatory inspections and grant applications. Technology transforms a manual chore into an automated safeguard.
Shelf-Life Management and Fourteen-Day Rotation Strategies
Whole blood remains viable for twenty-one days, yet wastage climbs after two weeks. Agencies rotate units to hospital stock on day fourteen and receive fresh replacements. Scheduled exchanges align with shift changes and never disrupt coverage. Consistent rotation maintains quality while keeping discard rates under five percent. Finance teams appreciate recovered value from hospital restocking.
Portable Warmers and Rapid Infusers for Field Use
Battery-powered warmers bring units to body temperature within ninety seconds. Inline pressure systems like LifeFlow deliver a full unit in under two minutes. Gauges prevent hemolysis by moderating flow despite vehicle jolts. Compact footprints fit crowded cabins without limiting patient access. Warmer whole blood preserves coagulation and fights hypothermia simultaneously.
| Cooler Model | Hold Time (hrs) | Capacity (units) | Tracking / Smart Features | Example Field Use |
|---|---|---|---|---|
| Crēdo ProMed | 72 – 96 | Up to 4 | Passive PCM; no telemetry | San Antonio FD rotation model |
| Delta ICE 2 L | 48 | 2 | Bluetooth + cellular temp logs | Widely used by U.S. EMS |
| Golden Hour | 72 | 1 – 4 | Modular VIP insulation | U.S. military tactical teams |
| 24-h Validated Compact Cooler* | 24 | 2 | No onboard telemetry | Australian helicopter EMS |
Operational Workflow on Scene
Inclusion Criteria and Decision Tree for Initiating Transfusion
Crews use quick checks: systolic pressure under ninety, penetrating torso wounds, or positive ultrasound. Cards mounted on monitors guide thumbs-up decisions in under ten seconds. Dispatch notes trigger hospital alerts so surgeons prepare operating rooms. Crews responsible for children schedule PALS renewal alongside weight-based transfusion training to sharpen pediatric airway and rhythm recognition. Rapid greenlights keep scene times tight and outcomes strong. Every minute saved boosts survival odds.
Step-by-Step Transfusion Procedure (Prep to Documentation)
Paramedics verify identity, spike the unit, and open flow wide for the first bolus. A second provider records lot numbers and cooler temperature before handing calcium gluconate. Continuous vitals watch for reaction signs while transport moves. On hospital arrival, crews hand off documentation and empty bags for chain-of-custody. The process balances speed and meticulous traceability.
Adjunct Medications: Calcium, TXA, and Damage-Control Resuscitation
Crews administer tranexamic acid within three hours to lock fibrin clots. Calcium replaces ions bound by citrate preservatives after the first unit. Permissive hypotension maintains forming clots without starving organs of perfusion. Whole blood, TXA, and calcium operate as a coordinated bundle. Damage-control strategies harmonize prehospital and surgical efforts.
Training and Competency Maintenance
Curriculum Design: Didactics, High-Fidelity Simulation, and Testing
Eight-hour courses blend clotting physiology with hands-on cooler drills and ambulance scenarios. Mannequins bleed in real time, demanding decisive interventions under flashing lights. Instructors debrief communication, gear placement, and documentation errors. ACLS certification refreshers fold into the eight-hour whole-blood course, reinforcing cardiovascular decision-making. Written exams then verify knowledge retention above ninety percent. Providers exit confident and protocol-fluent.
Continuing Education, Skills Validation, and QA Feedback Loops
Quarterly refresher labs revisit reaction management and new equipment updates. Quality-assurance teams review every transfusion within seventy-two hours for protocol drift. Dashboards share survival data, wastage rates, and documentation accuracy. Feedback sessions correct gaps before habits cement. Continuous learning keeps programs sharp and compliant. Quarterly drills also revise BLS for healthcare providers skills, ensuring compressions remain effective when blood alone cannot restore perfusion.
Data Collection, Outcome Tracking, and Continuous Improvement
Key Performance Indicators and Benchmark Metrics
Medical directors track time-to-blood, scene duration, twenty-four-hour survival, and adverse events. Dashboards compare local results against trauma registry averages and highlight emerging trends. Monthly reviews steer equipment upgrades and protocol tweaks. Data empowers improvement rather than fulfilling paperwork alone. Evidence becomes the program’s compass.
Reporting to Trauma Registries and Publishing Results
Agencies export anonymized datasets to state registries and multi-center studies. Peer-reviewed publications boost external credibility and unlock research grants. Transparent reporting earns public trust and keeps funders engaged. Shared data accelerates collective learning across regions. Collaboration turns isolated victories into national progress.
Cost, Reimbursement, and Long-Term Sustainability
Budgeting for Equipment, Supplies, and Wastage Mitigation
Startup budgets list coolers, warmers, training hours, and projected wastage. Finance officers weigh costs against reduced hospital length-of-stay and improved survivals. Rotation strategies recover unused units and soften spending spikes. Grant-writing teams highlight cost-to-benefit ratios when courting donors. Numbers tell a persuasive story.
Emerging CMS Billing Codes and Private-Payer Policies
Federal agencies consider bundled payments covering product, equipment, and staff time. Private insurers pilot contracts rewarding documented survival gains. Stable funding streams move programs from pilot to permanent status. EMS leaders track policy updates and adjust budgets accordingly. Financial health sustains clinical excellence.
Case Studies and Lessons From Early Adopters
Urban Deployment: Montgomery County, Maryland
Montgomery County stocked two units per ALS chase vehicle after six months of planning. Crews treated sixty-five patients during the first year with sixty-seven-percent survival. Four-percent wastage underscored efficient rotation schedules and data logging. Success prompted expansion to every frontline ambulance. Urban congestion no longer delayed lifesaving blood.
Rural Rollout: South-Carolina Rapid-Response Program
A rural South-Carolina agency placed coolers on supervisor trucks to counter helicopter delays. Twenty-three patients received whole blood in fields and farm roads with sixty-one-percent survival. Six-percent wastage remained below component-therapy averages despite long drives. Strategic placement maximized sparse resources. Rural geography proved no barrier to modern care.
Consortium Model: South-Texas STRAC Network
The South-Texas Regional Advisory Council united more than fifty services under a single donor pool. Central software balanced inventory, scheduled drives, and shared outcome dashboards. Three units per responder covered urban sprawl and border highways. First-year data showed sixty-nine-percent survival with three-percent wastage. Shared governance delivered scale and savings.
Challenges and Future Directions
Scaling Donor Supply and Cold-Chain Capacity Nationwide
Blood centers launch targeted drives and mobile buses to recruit low-titer donors. Manufacturers develop smart coolers that auto-adjust insulation to ambient conditions. Federal grants support rural distribution hubs and refrigerated drones. Expanding supply and transport technology must advance together. National coverage sits within reach.
Research Gaps: Optimal Ratios, Pediatric Use, Non-Trauma Indications
Scientists debate whether additional platelets enhance outcomes after multiple units. Formal pediatric trials will clarify dosing and reaction risks for smaller bodies. Investigators explore whole blood for obstetric hemorrhage and gastrointestinal bleeding. Broadening indications could amplify lives saved. Rigorous studies will guide evidence-based expansion.
Technological Innovations on the Horizon (Smart Coolers, Point-of-Care Typing)
Smart coolers stream live temperatures and battery status to command centers. Handheld spectrometers promise instant blood typing on crashed highways. Artificial-intelligence dispatch models position units near predicted high-risk events. Technology aims to slash time-to-blood even further. Tomorrow’s gear will refine today’s successes.
3 Practical Tips for Launching a Whole-Blood Program
- Pilot small and measure every metric: One cooler in a supervisor vehicle yields data to refine protocols before full scale.
- Rotate units back on day fourteen: Returning unused blood protects quality and keeps wastage under control.
- Embed simulation in monthly drills: Realistic practice cements muscle memory and reveals latent safety threats early.
FAQ: Prehospital Whole-Blood Essentials
What titer level qualifies as “low-titer” in civilian programs?
Most services label units low-titer when anti-A and anti-B antibodies test below 1:256. This threshold improves universal compatibility while keeping donor screening practical.
How do agencies handle transfusion reactions in the prehospital setting?
Crews stop infusion, administer antihistamines or epinephrine per protocol, and expedite hospital transport. Quality-assurance teams review events and adjust donor selection if patterns emerge.
Is LTOWB safe for pediatric trauma patients?
Early case reports suggest safety when crews calculate weight-based volumes. Ongoing clinical trials will establish formal pediatric guidelines and monitor rare complications.
What are the minimum documentation requirements for each transfusion?
Providers record cooler ID, lot number, start and stop times, vital signs, and medications. Complete logs support traceability, quality tracking, and future reimbursement claims.
Key Operational Takeaways for EMS Leadership
Evidence confirms whole blood saves lives when delivered quickly and logged meticulously. Successful programs rely on early stakeholder alignment, disciplined training, and transparent data dashboards. Reimbursement pathways and smart technology now lower financial and logistical barriers. Leaders who act decisively today position their communities for tomorrow’s strongest trauma survival rates.

Lisa VanderMeulen brings over 15 years of field experience as a licensed paramedic and firefighter in Florida. She currently serves as a Lieutenant with the Lehigh Acres Fire Control & Rescue District and as Dean of Ricky Rescue Training Academy, where she oversees curriculum development for EMT and fire service education.
Lisa holds an Associate of Science in Emergency Medical Services Technology from Florida SouthWestern State College and advanced certifications from the Florida Bureau of Fire Standards & Training, including Fire Officer II, Fire Instructor II, and Incident Safety Officer. Her licensure as a paramedic is backed by the Florida Department of Health.
In addition to her teaching and command roles, she actively serves on safety committees, community outreach programs like Fire Prevention Week and Pink Heals, and holds leadership positions within IAFF Local 1826.

