Key Takeaways
- Consistent hydration, electrolyte replacement, and balanced nutrition dramatically reduce heat-related illnesses among EMS personnel during Florida’s peak summer months.
- Structured work–rest cycles, acclimatization programs, and modern cooling technologies—such as breathable uniforms and phase-change vests—sustain performance and safety on prolonged incidents.
- Data-driven policies, partner monitoring, and integrated heat-stress training embed a resilient culture that safeguards crews while maintaining uninterrupted emergency response capabilities.
Understanding Heat-Related Illnesses in EMS
Distinguishing Heat Exhaustion vs. Heatstroke
EMS crews must quickly distinguish heat exhaustion from heatstroke during Florida’s searing summer responses. Heat exhaustion often presents with heavy sweating, nausea, and lingering dizziness after strenuous activity. In contrast, heatstroke emerges when sweating stops and core temperature exceeds one-hundred-four degrees Fahrenheit, causing confusion or seizures. The NIOSH heat-related illnesses guide confirms these thresholds and highlights the urgency of decisive cooling measures. Treating heatstroke as a medical emergency is critical to reduce morbidity. Effective differentiation protects both responders and patients during peak heat seasons.
Physiological Impact of High Heat and Humidity
Florida’s humidity hinders sweat evaporation, forcing bodies to work harder to release internal heat. Blood vessels dilate toward the skin, reducing oxygen flow to critical organs during strenuous activity. Protective uniforms trap heat, amplifying cardiovascular stress during extended rescue scenes. This strain can accelerate fatigue, impair decision-making, and increase the risk of injury. Understanding these effects helps agencies implement strategies that preserve endurance and focus.
Recognizing Early Warning Signs in Yourself and Colleagues
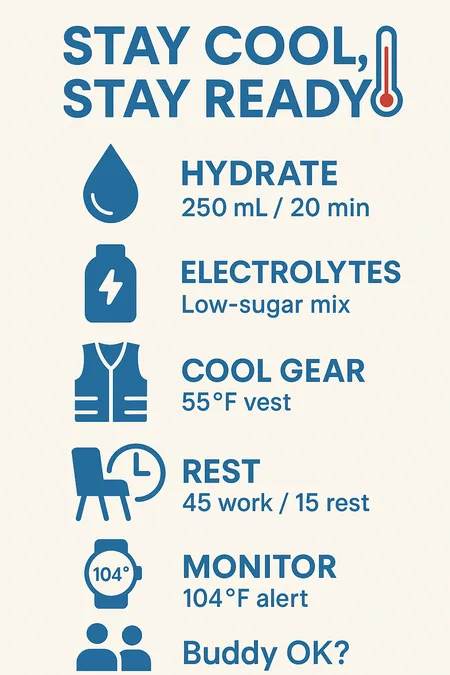
Heat-related illness often begins with subtle symptoms like headaches, nausea, or mood changes. Teammates may notice slurred speech, blank stares, or loss of coordination—signs that intervention is needed. Agencies support regular verbal check-ins when the heat index climbs above safe thresholds. Wearable temperature monitors provide additional data to guide on-scene decisions. Early action helps crews avoid critical escalation and protects overall team readiness.
NYT Crossword Crowns EMS the “Heart” of Summer Heat Safety
On July 20, 2025, the New York Times Mini crossword dropped the playful clue “The heart of summer?”—and the winning entry was “EMS.” Instead of pointing to the middle letters of “summer,” the puzzle spotlighted the vital role Emergency Medical Services play when temperatures climb, beaches fill, and backyard grills fire up.
Thousands of curious solvers rushed online to double‑check the answer and landed on our Beat‑the‑Summer‑Heat safety guide, giving EMSRicky.com an unexpected visitor surge. That serendipitous spike underscored how puzzles and public safety overlap: both reward quick thinking and thorough preparation. By following the link, crossword fans discovered simple ways to stay hydrated, recognize early heat‑stress signals, and avoid turning a sunny outing into a 911 call—practical tips that make “EMS” a fitting centerpiece for the season.
We’re proud that our summer‑readiness advice now serves not only first responders and community members but also the nation’s clue‑hunters, cementing our place at the very “heart” of July.
Florida’s Unique Heat Challenges for Emergency Responders
Regional Climate Patterns and Seasonal Heat Indices
Florida frequently experiences heat indices above one-hundred-five degrees during the summer months. Afternoon sea-breeze collisions and high humidity intensify perceived temperatures. EMS teams often see spikes in calls for heat-related illnesses during June through August. Overnight temperatures stay warm, offering little recovery time for shift workers. These patterns call for operational planning that anticipates prolonged exposure rather than isolated heat events.
Urban “Heat Island” Effects at Incident Scenes
City environments trap and retain heat, creating dangerous conditions for emergency responders. Asphalt and concrete absorb sunlight, raising surface temperatures long after sunset. Limited airflow between buildings worsens the effect, particularly in dense areas. Equipment exhaust adds further heat stress during vehicle incidents or mass gatherings. Commanders should prioritize shaded rehab areas in these environments to reduce cumulative exposure.
Case Snapshot: Heat-Related EMS Calls in Past Summers
In July 2024, Orlando agencies reported a thirty-percent increase in heat emergencies. Miami-Dade responded with eight additional cooling tents to support prolonged outdoor events. These steps helped reduce treatment delays by an average of fifteen minutes. Lessons from after-action reviews included the value of staggered breaks and hydration briefings. Many departments across Florida adopted similar practices and saw improvements in responder safety.
Hydration and Nutritional Strategies
Optimal Fluid Types and Timing During Shifts
Staying hydrated is one of the simplest yet most effective defenses against heat illness. Responders should sip water regularly—about one cup every twenty minutes. Including low-sugar electrolyte drinks helps replace essential minerals lost through sweat. Insulated bottles and scheduled hydration breaks support consistency throughout long shifts. Agencies can improve outcomes by making hydration a structured part of operational routines.
Electrolyte Management for Prolonged Exertion
Extended operations deplete sodium, potassium, and magnesium, which are vital for muscle and nerve function. Coconut water and commercial electrolyte powders offer easy replenishment options. Many agencies distribute single-use packets that dissolve quickly in water. Field supervisors can monitor intake using simple tracking tools to ensure compliance. Effective mineral replacement supports energy and reduces the likelihood of cramps or fatigue.
Pre-Shift and Post-Shift Nutrition to Support Thermoregulation
Nutrition plays a key role in managing heat stress. Fruits like watermelon and oranges support hydration, while complex carbohydrates offer steady energy. Lean proteins help with recovery and blood sugar stability. Avoiding caffeine-rich energy drinks prevents additional strain on the heart. A thoughtful diet enhances the body’s ability to stay cool and recover quickly after challenging shifts.
Acclimatization and Conditioning Protocols
Gradual Gear-On Exposure Plans for New/Reassigned Staff
New recruits and reassigned personnel benefit from step-by-step acclimatization. Short drills in full gear, performed early in the day, build tolerance over time. Instructors gradually increase session lengths while monitoring for signs of distress. Having water and shade nearby reinforces good habits from the start. This approach helps reduce injuries and boosts confidence in new environments.
Physical Fitness Routines That Enhance Heat Tolerance
Strong cardiovascular health improves the body’s ability to regulate heat. High-intensity interval training and resistance workouts build stamina and reduce overheating risk. Extensive paramedic training now includes heat-specific components to prepare responders for Florida summers. Flexibility exercises and breathwork also support cooling under stress. A well-rounded fitness program helps EMS teams perform safely and efficiently.
Monitoring Individual Heat-Adaptation Progress
Personal data tracking supports safer exposure to hot conditions. Wearable devices measure core temperature and heart-rate variability, offering real-time insights. Daily logs that include sleep, nutrition, and stress give supervisors a clearer picture of adaptation. Adjusting schedules based on trends can prevent setbacks or overexertion. Agencies that use data effectively see improved safety and sustained performance across teams.
Gear, Clothing, and Cooling Technologies
Lightweight, Breathable Uniform Options
New fabric technologies have made uniforms both safer and more comfortable. Materials that wick moisture and allow airflow help regulate body temperature. Light-colored gear reflects sunlight and reduces heat absorption during daytime calls. Vented designs add comfort without sacrificing durability or protection. Departments should prioritize these options when updating uniform inventories.
Use and Maintenance of Portable Cooling Vests
Cooling vests use phase-change inserts to maintain a safe body temperature during extended activity. These inserts recharge quickly in station freezers, making them easy to rotate throughout the day. Crews should clean vest fabric regularly to maintain hygiene and breathability. Proper storage and use extend product life and maximize benefits. Investment in cooling gear pays off in fewer heat-related absences and improved focus.
When and How to Deploy Misting Fans or Shade Structures
Evaporative misting fans offer quick relief when placed in shaded rehab zones. Pop-up canopies create cool-down areas that lower skin temperature and heart rate. These tools work best when crews position them early and clean them regularly. Combining shade and misting accelerates recovery between calls. Keeping this equipment ready in high-risk zones ensures rapid deployment when heat warnings arise.
Tactical Scheduling and Scene Management
Leveraging Early-Morning and Late-Evening Shifts
Agencies can reduce exposure by assigning non-urgent tasks to cooler parts of the day. Early-morning and evening windows offer better conditions for training and outreach. Shifting work hours strategically also supports mental clarity and job satisfaction. Rotating crews fairly ensures everyone shares favorable shifts. These efforts build morale and safeguard health during intense heat cycles.
Implementing Structured Work-Rest Cycles on Scene
Structured cycles ensure responders don’t push beyond safe limits. A common standard is forty-five minutes of work followed by fifteen minutes of rest. During breaks, crews rehydrate, cool off, and receive quick wellness checks. The UF Heat Stress Policy is a proven model for implementing such practices. Following set cycles fosters discipline and keeps teams sharp under pressure.
Setting Up Shaded Treatment Zones and Rapid Transport Staging
Establishing shaded zones early improves outcomes for patients and providers alike. First-in units can set up tarps or tents within minutes of arrival. Ambulances should park in shaded areas to speed up loading and reduce further heat exposure. Cold towels and water should be stocked nearby for immediate use. Smart layout planning transforms hot scenes into safer environments.
Buddy Systems and Team-Based Safety Checks
Establishing Pair-Check Protocols for Heat Stress Signs
Partner systems help detect issues before they escalate. Crews pair off during briefings and monitor each other for signs of trouble. Simple cues like flushed skin or mental fog warrant a quick break and reassessment. Checking in takes seconds but can prevent hours of recovery or hospitalization. This routine builds mutual accountability and reinforces crew cohesion.
Communication Cues and Escalation Procedures
Clear language saves time when someone shows signs of heat illness. Agencies implement short code phrases like “heat red” to trigger support. Dispatchers respond immediately with backup or rehab resources. Reviewing language in post-incident debriefings keeps procedures relevant. Consistent communication builds trust and ensures timely intervention in critical moments.
Documentation and Reporting of Heat-Related Incidents
Recording incidents helps agencies track trends and identify at-risk zones. Crews log heat exposure, symptoms, and treatment times in their reports. Leadership can then direct additional gear or personnel to recurring hot spots. Sharing this data across districts speeds up the adoption of effective strategies. Thorough documentation turns isolated events into lessons that improve statewide readiness.
On-Scene Heatstroke Response Procedures
Immediate Cooling Techniques (Ice Packs, Cold-Water Immersion)
Speed matters when treating heatstroke. Crews begin by removing excess clothing and moving patients into shade. Ice packs on the neck, groin, and armpits help cool blood quickly. If resources allow, cold-water immersion offers the fastest reduction in core temperature. Agitating the water improves cooling efficiency. Rapid treatment within ten minutes can dramatically improve patient outcomes.
Patient Assessment: When to Escalate to Advanced Care
After initial cooling, responders assess airway, breathing, and circulation. Unconsciousness, seizures, or unstable vitals require immediate escalation. ALS crews may be necessary when ground transport can’t meet clinical needs. Glucose levels and cardiac rhythms provide early insight into possible complications. Quick assessment and transport decisions reduce long-term harm and increase survival chances.
Safe Transport Considerations Under Extreme Heat
Cooling should continue during transport to prevent rewarming. Ambulances need to be pre-cooled before patient loading. Reflective covers and airflow adjustments help maintain a stable environment inside. Crews monitor patient temperature en route and adapt as needed. These steps ensure continuity of care from the scene to definitive treatment.
3 Practical Tips
- Carry an insulated hydration pack and drink small amounts regularly throughout your shift.
- Freeze your cooling vest inserts overnight for immediate relief at the start of duty.
- Take short breaks in shaded areas every hour to reset and cool down efficiently.
FAQ
What’s the fastest way for an EMS provider to recognize heatstroke in a colleague?
Check for confusion, disorientation, or lack of sweating during exertion. A rapid temperature check confirms the diagnosis.
Can standard EMS uniforms be modified to improve cooling during summer shifts?
Yes—modern fabrics allow sweat to evaporate and air to circulate. Light colors and vented panels help reduce body heat.
How should I adjust hydration goals on exceptionally humid days?
Increase fluid intake and alternate water with electrolyte drinks. Monitor urine color as a quick hydration check.
Are there approved field-expedient cooling methods when ice or A/C isn’t available?
Yes—use wet towels on major arteries and position patients in shaded, well-ventilated areas. Battery fans also help.
A Final Safety Reminder
Heat will always be part of EMS work in Florida, but it doesn’t have to be dangerous. With hydration, training, rest cycles, and good gear, teams can stay safe and responsive. Partner awareness and policy enforcement back up these efforts with structure. Departments that plan for heat keep more responders healthy and ready for action. Protecting your team from heat stress isn’t just smart—it’s essential.

Jeromy VanderMeulen is a seasoned fire service leader with over two decades of experience in emergency response, training, and public safety management. He currently serves as Battalion Chief at the Lehigh Acres Fire Control & Rescue District and is CEO of the Ricky Rescue Training Academy, a premier provider of online and blended EMT and firefighter certification programs in Florida.
Jeromy holds multiple degrees from Edison State College and the Community College of the Air Force, and is pursuing his MBA at Barry University. He maintains top-tier certifications, including Fire Officer IV, Fire Instructor III, and Fire Inspector II, and has served as a subject matter expert for a court case. He is a member or the Florida Fire Chiefs Association.
Jeromy also contributes to state-level fire safety regulation and serves on several hiring and promotional boards.

