Key Takeaways
- Fireworks events pose unique EMS challenges due to crowd density, blast injuries, and limited access—requiring pre-positioned units and burn-specific gear.
- Effective response depends on clear triage protocols, pediatric-specific care plans, and rapid activation of ALS or air medical support when needed.
- Community safety improves when EMS participates in multi-agency planning, delivers tailored public education, and tracks injury data for future prevention.
Understanding the Scope of Fireworks-Related Injuries
Why July Events Pose a Unique EMS Challenge
Independence-month celebrations compress thousands of displays into long holiday weekends, creating simultaneous medical hot spots. Crowded venues and heavy traffic extend travel times, so EMS units must stage closer than usual. Alcohol consumption and relaxed supervision elevate risk-taking with fireworks, pushing minor mishaps toward major trauma. Weather adds complexity because summer heat worsens dehydration and smoke visibility challenges. Coordinated preparation offsets these predictable stressors and keeps fireworks safety for EMS manageable.
Common Injury Types Linked to Fireworks Use
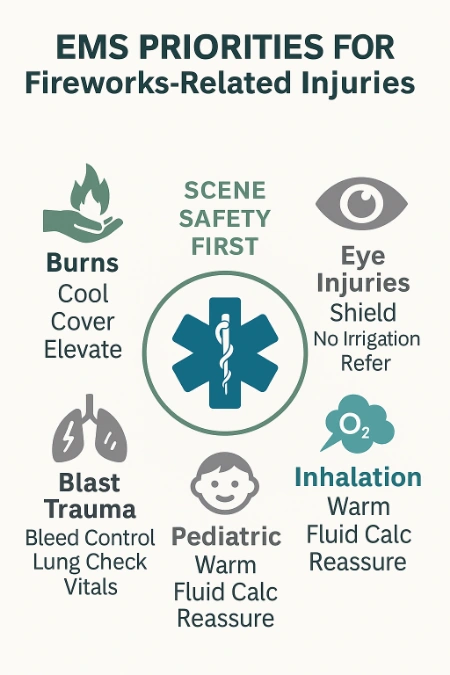
Burns dominate call volumes, yet blast trauma often carries the greatest mortality risk. Hands, face, and eyes suffer when shells misfire or users lean over tubes. Fragment injuries create deep lacerations and partial amputations that demand rapid hemorrhage control. Smoke inhalation and tympanic membrane rupture emerge when spectators crowd launch zones. Recognizing this pattern guides supply lists and triage priorities.
Age Groups and At-Risk Demographics
Children sustain sparkler burns because parents overlook lingering metal temperatures of 1,800 °F. Teenagers experiment with homemade mortars, accounting for most blast-related hand injuries. Older adults experience severe facial trauma because slower reflexes delay evasive movement. Families in dense housing often ignite fireworks near obstacles, amplifying ricochet risks. Tailored outreach that targets each demographic reduces preventable damage.
Pre-Event EMS Strategy and Coordination
Working with Event Organizers and Local Authorities
EMS leaders attend permit meetings to map launch pads, fallout corridors, and medical posts. Input from medics influences barricade placement, signage wording, and radio channel assignments. Clear memoranda establish who authorizes show delays when wind shifts threaten spectators. Vendor placement and food-truck propane storage also receive medical oversight. Collaboration eliminates confusion once crowds arrive.
ICS Integration and Role Assignment
Unified command structures prevent redundant orders and streamline multi-agency communication. A medical branch director tracks patient flow while a logistics officer manages resupply. Triage group supervisors rotate fatigued personnel, sustaining peak performance through extended events. Clear titles and vests help other agencies identify decision-makers instantly. Training together before July guarantees muscle memory under pressure.
Pre-Positioning Units for Rapid Access and Egress
Ambulances park outside crowd pinch points, facing outbound lanes for swift departure. Bicycle medics patrol dense zones, shrinking response times where vehicles cannot reach. UTV crews shuttle equipment across uneven fields without jostling victims. Dedicated ingress and egress lanes remain coned and patrolled to deter tailgaters. Strategic staging preserves precious minutes when multiple patients surface simultaneously.
Essential Supplies and Burn-Specific Gear Checklist
Every fireworks detail kit carries abundant burn sheets, water-based gel, and sterile saline liters. Eye shields, tourniquets, and hemostatic gauze sit on top for instant reach. Flame-resistant blankets smother embers that cling to synthetic clothing. Ear protection minimizes responder fatigue near launch cannons. Pre-event inventory checks ensure nothing expires mid-mission.
Scene Entry Protocol and Hazard Assessment
Identifying Active and Latent Scene Dangers
Crew leaders halt at a safe distance, scan wind direction, and locate unspent shells. Smoldering grass, propane cylinders, and hanging power lines influence the approach path. Thermal imaging cameras reveal hidden hotspots in tall debris piles. Cones mark danger zones to keep helpers from wandering into hazards. A deliberate entrance protects patients and responders alike.
RAT Protocol: Rapid Assessment for Fireworks Incidents
Recognize threats first, activate extra resources second, treat victims third—always in that order. Spotting cracked mortars or leaking fuel justifies calling hazmat or ladder companies immediately. Treatment begins only when responders trust the environment. This disciplined flow shortens scene time while preserving safety. RAT keeps crews mission-focused amid sensory overload.
Securing the Scene from Crowd Interference
Barrier tape and human shields carve treatment corridors free of spectators. Public-address announcements calm anxious families and direct them toward reunification tents. Volunteers distribute water to curb heat agitation among onlookers. Visible boundaries discourage smartphone filming that blocks stretcher routes. Orderly perimeters allow medics to concentrate on lifesaving tasks.
Initial Triage and Life-Saving Priorities
Airway, Breathing, and Circulation in Firework Trauma
Facial burns swell rapidly, so airway equipment must stand ready during assessment. High-flow oxygen counters inhalation injury while responders monitor carbon-monoxide saturation. Direct pressure and commercial tourniquets stop arterial bleeding within seconds. Intravenous fluids maintain perfusion when burns exceed ten percent body surface area. Continuous reassessment detects subtle deterioration before it turns irreversible.
Rapid Neurological Evaluation and Burn Surface Area Estimation
Glasgow Coma Scale scoring uncovers blast concussions that demand trauma center care. The Rule of Nines or Lund-Browder charts calculate fluid replacement needs precisely. Accurate numbers prevent under-resuscitation and tissue ischemia. Documenting depth and location supports transfer reports and surgical planning. Quick, precise data collection improves outcomes.
When to Call for ALS Support or Air Medical Evacuation
Airway burns requiring intubation or major amputations above the wrist justify ALS activation, especially when advanced cardiovascular life support is needed. Multisystem blast injuries and remote rural sites trigger helicopter requests without delay. Clear criteria limit debate during chaotic minutes. Early notification readies burn and trauma teams before wheels hit pads. Fast escalation saves limbs and lives.
Managing Common Fireworks Injuries
Burns: Cooling, Dressing, and Fluid Management
EMS crews cool burns with tepid water for ten minutes, stopping thermal spread. Rings, belts, and shoes come off before swelling traps them. Non-adherent dressings cover wounds, and limb elevation reduces throbbing pain. Burns over ten percent receive warmed crystalloids following Parkland guidelines. Analgesia begins en route to shorten hospital-door-to-debridement time.
Traumatic Amputations and Blast Injuries
Tourniquets tighten above the injury, achieving hemorrhage control in under one minute. Amputated parts receive saline rinse, moist gauze wrap, and secondary bagging on ice. Analgesics lessen sympathetic surges that worsen bleeding. Overpressure injuries may bruise lungs, so pulse oximetry tracks hidden hypoxia. Coordinated packaging preserves digits for reattachment.
Facial and Ocular Trauma Considerations
Rigid eye cups shield globes without applying pressure. Responders avoid ointments that cloud ophthalmologic inspection or trap residual heat. Gentle suction clears nasal bleeding that can obstruct airways. Airway tools stay near because facial burns often progress swiftly. Protecting vision and ventilation remains the dual priority.
Hearing Loss, Shockwave Injuries, and Inhalation Damage
Tympanic membrane rupture hints at internal barotrauma requiring hospital evaluation. Upright positioning reduces ear pain and discourages Valsalva attempts. Crew members auscultate lungs for diminished sounds suggesting contusion. Persistent coughing or sooty sputum prompts bronchodilators and early advanced care. Quick action curtails secondary complications.
This chart summarizes common fireworks-related injuries, their causes, and what EMS professionals should prioritize during on-scene care. Use it as a quick-reference guide to streamline field response during high-volume events.
| Injury Type | Typical Cause | EMS Field Priorities |
|---|---|---|
| Hand Burns | Improper handling of mortars or relighting duds | Cool with tepid water, remove jewelry, apply sterile dressing, assess for deeper trauma |
| Eye Injuries | Flying debris, shell explosions, or close-range sparklers | Shield with eye cup, avoid pressure or irrigation, prepare for rapid ophthalmologic referral |
| Blast Injuries | Improvised fireworks or shell failure | Control bleeding, check lung sounds, monitor for shock and airway compromise |
| Facial Burns | Close-range ignitions or unexpected shell trajectories | Secure airway early, apply dry sterile dressing, monitor swelling and saturation |
| Inhalation Injuries | Dense smoke from displays or clothing fires | Administer high-flow oxygen, monitor airway, prepare for advanced airway if needed |
Field Treatment Protocols for Pediatric Victims
Burn Response in Children: Fluid Resuscitation Guidelines
Children lose heat quickly, so ambient warmth matters during burn cooling. Parkland calculations remain weight-based, with dextrose added for neonates. Crews monitor glucose levels to dodge hypoglycemic surprises. Gentle verbal reassurance distracts young minds from frightening surroundings. Medics treating pediatric burn injuries benefit from staying current with PALS renewal standards to align care with the latest protocols.
Emotional Stabilization and Guardian Communication
Calm voices, eye-level positioning, and simple explanations lower cortisol surges in kids. Guardians help hold hands, providing comfort and behavioral cues. Crew members outline every step so parents feel included rather than helpless. Good communication reduces resistance during IV placement or dressing changes. Cooperative children speed scene clearance.
Age-Specific Equipment and Packaging Considerations
Pediatric airway adjuncts, cervical collars, and blood-pressure cuffs must fit snugly. Small burn sheets prevent multilayer bunching that causes pressure sores. Vacuum mattresses cradle toddlers without sliding during transport. Regular equipment inspections verify nothing expired or misplaced. Right-sized tools equal right-sized care.
Effective On-Site Crowd Management
Establishing Buffer Zones and Medical Corridors
Metal barricades and clearly painted stripes mark safe distances from launch sites. Directional arrow signs guide spectators toward aid posts. High-visibility medic vests reassure crowds and deter breach attempts. Dedicated corridors keep stretchers rolling without weaving. Organized spaces translate into faster interventions.
Managing Intoxicated Spectators and Bystander Surge
Joint patrols of medics and officers quell rowdy behavior before tensions escalate. Short, respectful commands steer impaired individuals away from hot zones. Hydration tents combat heat exhaustion that mimics alcohol effects. Controlled release of crowd sections prevents bottlenecks during evacuation. Active management keeps the scene peaceful.
Using Spotters and Barriers for Scene Safety
Elevated spotters scan for drifting sparks or shifting crowd density. Real-time radio updates redirect resources where pressure mounts. Flexible fencing expands or shrinks perimeters as conditions change. Distance-marker flags help families gauge safe viewing spots without constant announcements. Layered observation safeguards everyone present.
Post-Show Site Security and Cleanup Hazards
Handling Misfires and Unexploded Ordnance
Every dud shell remains dangerous until licensed technicians inspect it. Perimeter tape extends fifty feet beyond suspected devices. Fire extinguishers remain handy for sudden ignition events. GPS tagging of debris supports daylight retrieval. Patience beats bravery in unexploded ordnance handling.
Fire Watch Responsibilities and PPE Requirements
Thermal imagers detect hidden embers in grass or fencing materials. Fire-resistant coats, goggles, and nitrile gloves protect responders during debris sweeps. Pre-filled backpack sprayers extinguish mini-flare-ups instantly. Scheduled hydration breaks prevent heat-stroke among cleanup crews. Appropriate gear extends safety beyond the final burst.
Coordination with Fire and Law Enforcement for Debris Management
Unified command staggers cleanup crew entry to avoid chokepoints. Law enforcement secures exits while tow trucks clear vendor trailers first. Firefighters flush launch tubes before dismantling racks. EMS stands ready for minor sprains or burns that occur during takedown. Cooperative efforts close the night smoothly.
EMS Roles in Community Fireworks Safety Education
How to Deliver Public Safety Messaging Before Major Events
Short live-stream demonstrations reach residents who scroll social media daily. Radio interviews share designated viewing zones and traffic tips. Bilingual flyers at grocery stores connect with households lacking internet access. Consistent messaging across platforms amplifies retention. Preventive education trims incident numbers before they start.
Common Misconceptions about “Safe” Fireworks
Sparklers burn hotter than blowtorches, yet many parents treat them like glow sticks. “Re-light” instructions printed on packaging contradict best-practice guidelines and invite burns. Real injury photos—cropped to stay respectful—illustrate these dangers effectively. Data alone rarely change behavior; relatable stories succeed. Myth busting saves fingers and eyes.
Partnering with Schools, Media, and Fire Departments
Science-lab demonstrations help students visualize rapid tissue damage at high temperatures. Journalists publish interactive infographics comparing firework heat to everyday appliances. Fire departments loan inert shells for classroom show-and-tell. Multi-platform storytelling accommodates diverse learning styles. Partnership transforms passive audiences into proactive safety ambassadors.
FAQ: Fireworks Injuries and EMS Protocol
What’s the first priority when treating a fireworks burn injury?
Stop the burning process through gentle cooling that avoids ice or frigid water. Then apply sterile, non-adherent dressings and assess for additional trauma.
How should EMS handle unexploded fireworks at a scene?
Create a secure perimeter around the device and notify bomb technicians immediately. Keep bystanders clear until specialists confirm safety.
What crowd control methods work best at fireworks displays?
Clearly marked buffer zones paired with visible medical staff reduce pushing during emergencies. Advance messaging about exits encourages orderly movement if evacuation occurs.
When should a fireworks-related injury be considered a trauma alert?
Activate trauma teams for airway burns, multi-system blast injuries, or amputations above the wrist or ankle. Early alerts prepare surgeons and burn specialists for rapid intervention.
3 Practical Tips for EMS Crews at Fireworks Events
Always Keep Burn Gel and Dry Sterile Dressings Within Reach
A separate burn pouch prevents digging through crowded compartments when seconds matter. Crews check expiration dates weekly during fireworks season. Organized supplies translate into swift pain relief. Quick cooling limits tissue destruction. Efficient packaging streamlines restocking.
Position Units to Avoid Getting Boxed In by Crowd Movement
Parking near exit gates ensures ambulances escape post-show gridlock. Drivers face outward to eliminate complex reversals under stress. Bicycle medics scout terrain for congestion warnings. Real-time updates let command reroute resources proactively. Mobility equals survivability for patients.
Have a Pre-Briefed Plan for Pediatric Victim Handling
Assign one medic as family liaison to keep guardians informed and calm. Child-sized oxygen masks and distraction toys ride in a dedicated pediatric pouch. Crews rehearse loading small stretchers smoothly onto cots. Confidence grows when every member knows specific roles. Prepared teams soothe young patients quickly.
Looking Ahead: Reducing Fireworks Injuries Through Better EMS Integration
Post-Incident Data Collection and Reporting Improvements
Standardized after-action forms capture device type, distance, and protective measures. Uploading data to regional registries reveals trends that guide next year’s prevention strategies. Transparent reporting convinces policymakers to tighten safety ordinances where gaps exist. Evidence drives meaningful change. Precise numbers save futures.
Event Debriefs: What Went Well and What Needs Change
Hot-wash sessions within twenty-four hours preserve vivid memories and honest feedback. Facilitators categorize comments into keep, fix, and try buckets for actionable outcomes. Sharing lessons with neighboring agencies multiplies improvements across counties. Incremental adjustments accumulate into substantial risk reduction. Open dialogue fuels progress.
Building Multi-Agency Response Models for Annual Recurring Events
Year-round planning committees integrate lessons into updated protocols. Tabletop exercises and live drills stress-test new ideas under simulated fireworks conditions. Community advisors contribute cultural insights that refine messaging and volunteer coordination. Unified models create predictable workflows every summer. Sustained collaboration keeps celebrations bright and safe.
Community celebrations stay joyful when EMS teams prepare, educate, and respond with decisive expertise.

Jeromy VanderMeulen is a seasoned fire service leader with over two decades of experience in emergency response, training, and public safety management. He currently serves as Battalion Chief at the Lehigh Acres Fire Control & Rescue District and is CEO of the Ricky Rescue Training Academy, a premier provider of online and blended EMT and firefighter certification programs in Florida.
Jeromy holds multiple degrees from Edison State College and the Community College of the Air Force, and is pursuing his MBA at Barry University. He maintains top-tier certifications, including Fire Officer IV, Fire Instructor III, and Fire Inspector II, and has served as a subject matter expert for a court case. He is a member or the Florida Fire Chiefs Association.
Jeromy also contributes to state-level fire safety regulation and serves on several hiring and promotional boards.

