Key Takeaways
- Summer crowding and alcohol raise drowning risk, so data-driven staffing and prevention messaging become essential.
- Rapid airway clearance, hypothermia management, and ACLS-level skills boost survival after water-related cardiac arrest.
- Cross-trained agencies, staged equipment, and regular shoreline drills transform chaotic scenes into coordinated, efficient rescues.
Understanding Seasonal Risk: Why Summer Brings a Surge in Water Emergencies
Summer heat draws crowds to water, so incident numbers surge across beaches, lakes, and pools, as confirmed by a CDC study. Data from previous seasons helps EMS leaders position units near repeating hotspots before crowds arrive. Extended daylight encourages longer outings, and alcohol consumption rises, so vigilance must intensify accordingly. Teams adjust staffing patterns based on tourism calendars, school breaks, and local festival schedules. Public-health partners share demographic insights, letting educators tailor prevention messages toward children, teens, and older adults. Early, targeted outreach consistently decreases call volume, while improving community trust in prehospital services.
Common Water-Related Emergencies EMS Teams Face
Drowning and Near-Drowning Incidents
Submersion deprives the brain of oxygen within minutes, so rescuers prioritize airway management immediately. Crews practice inline spinal stabilization alongside ventilation drills during monthly training sessions. Near-drowning victims might seem stable, yet delayed pulmonary edema can appear hours later, a finding detailed in an NCBI review. Medics therefore recommend hospital observation even when initial examinations look reassuring. Prompt oxygenation and continuous monitoring improve neurological outcomes across all age groups. Consistent protocols protect clinicians from hesitation and patients from secondary complications.
Boating and Jet Ski Accidents
High-speed impacts often fracture vertebrae, so responders approach every boating collision with spinal precautions. Crews secure flotation collars and slide victims onto backboards before moving toward shore. Spilled fuel, spinning propellers, and unpredictable wakes create secondary hazards that demand strict scene control. Marine patrol officers enforce safety zones, while EMS maintains direct radio contact to coordinate extraction. Quick, clear communication prevents additional crashes and expedites definitive trauma care. Prepared teams convert chaotic waterways into organized treatment corridors within minutes.
Environmental Hazards and Submersion Risks
Rip currents pull swimmers seaward rapidly, so beach units drill diagonal rescue approaches weekly. Swift-water teams contend with submerged debris and murky visibility, requiring sharp situational awareness. United States beaches record roughly one hundred rip-current deaths each year, according to NOAA data. Cold-water shock can paralyze breathing muscles even on hot days, complicating resuscitation efforts. Responders initiate hypothermia protocols immediately, including foil blankets and warmed IV fluids. Thunderstorms bring lightning risks; therefore supervisors evacuate crews once strikes occur within ten miles.
Scene Safety and Initial Risk Assessment
Responders perform 360-degree scans before committing resources to any aquatic scene. They favor reach-or-throw methods until specialized swimmers or divers arrive with proper support. Incident commanders assign lookouts to track changing currents, approaching vessels, and incoming weather fronts. Clear role assignments using standardized hand signals reduce miscommunication in noisy environments. Triaging multiple victims starts with unconscious patients while conscious swimmers receive flotation and verbal reassurance. Strong safety culture protects rescuers and preserves resources for prolonged operations.
Pre-Arrival Preparedness and Team Readiness
Specialized Training for Aquatic Response
Muscle memory fades without repetition, so agencies schedule quarterly water-rescue drills in varied settings. Medics practice breath-controlled dives, patient rollovers, and spine-secure lifts until movements feel automatic. Cross-training with lifeguards and firefighters builds trust and unifies terminology. Shared exercises expose equipment gaps before real incidents expose them under pressure. Instructors review performance metrics afterward and assign targeted skill refreshers. Regular, realistic training maintains confidence and accelerates future rescues.
Equipment That Saves Seconds
Crews stage throw bags, rescue boards, and flotation vests near ambulance side doors for immediate access. Waterproof cardiac monitors and insulated AED pads enable safe shoreline defibrillation without dangerous arcing. Portable suction units clear airways quickly, minimizing hypoxic injury. Compact hypothermia wraps and chemical heat packs stabilize core temperatures during transport. Regular inventory checks ensure batteries remain charged and straps stay functional. Strategic equipment placement converts seconds saved into lives saved.
Working with Marine and Lifeguard Units
Overlapping jurisdictions require clear agreements long before peak season begins. Agencies establish unified radio channels and shared mapping platforms during winter planning sessions. Tabletop drills reveal terminology conflicts and equipment incompatibilities in advance. Dispatchers then route specialized divers or helicopter hoists without confusion. Respectful collaboration fosters seamless multi-agency operations when emergencies strike crowded waterways, especially when team leaders complete advanced paramedic courses.
Airway, Breathing, and Circulation: EMS Resuscitation in Water Emergencies
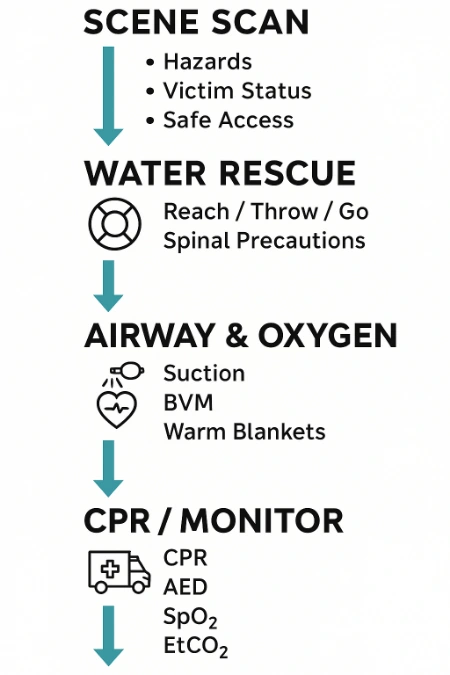
Water or vomit often obstructs oxygen exchange, so responders clear airways immediately after extraction. Medics position patients laterally, suction aggressively, and deliver bag-valve ventilations within the first minute, a core skill refined during ACLS certification training. Chest compressions require firm support, so teams use backboards or boat decks until reaching shore. Hypothermia hides pulses, so crews continue resuscitation until core temperatures exceed ninety-five degrees Fahrenheit. Warmed IV fluids, heated ambulance cabins, and chemical packs raise body temperatures steadily. Continuous EtCO₂ monitoring guides ventilation quality and signals early return of spontaneous circulation.
Transport, Handoff, and Hospital Communication
Definitive care starts at the hospital, so medics deliver concise, thorough handoffs en route. They report submersion duration, water temperature, initial Glasgow scores, interventions, and observed complications. Secure channels allow continuous vital sign updates, letting emergency departments mobilize respiratory teams early. Smooth transitions maintain ventilation support and therapeutic warming without interruption. Effective communication bridges prehospital efforts and in-hospital treatments, protecting neurological outcomes. ED staff appreciate detailed field data, which accelerates imaging, lab work, and definitive airway decisions.
Post-Rescue Observation and Delayed Onset Complications
Fluid aspiration can cause delayed respiratory failure, so clinicians monitor survivors for twenty-four hours. Families receive education about warning signs like persistent cough, chest discomfort, or rapid breathing. Pediatric patients face higher risk because smaller airways swell quickly after irritation. Medics advocate hospital admission for children even when they appear playful on scene, advice reinforced through regular PALS renewal programs. Early recognition and observation prevent tragic reversals long after beaches empty.
This table presents specific symptoms that may signal post-rescue complications in near-drowning or submersion victims. EMS providers can use it as a quick guide to prioritize transport, observation, or escalation based on real-time patient presentations.
| Symptom | Possible Complication | EMS Response |
|---|---|---|
| Persistent cough | Secondary drowning or lung irritation | Recommend transport and ER observation |
| Low oxygen saturation | Impaired gas exchange due to aspiration | Administer oxygen; monitor SpO₂ closely |
| Confusion or lethargy | Ongoing hypoxia or possible head injury | Secure airway; initiate advanced assessment |
| Cool, pale skin | Hypothermia following immersion | Initiate active rewarming en route |
| Vomiting or coughing up foam | Pulmonary edema or aspiration | Position laterally; prepare for suctioning |
Community Engagement and Prevention: EMS Role Beyond the Rescue
Prevention efforts yield the greatest impact, so EMS educators visit schools and marinas before summer. They demonstrate proper life-jacket fitting, rip-current escape techniques, and CPR certification skills that empower bystanders. Short social-media videos showcase throw-bag rescues and poolside emergency plans, reaching busy parents. Local businesses sponsor signage that reminds patrons to swim sober and supervise children constantly. These campaigns reduce call volumes while strengthening community appreciation for first responders. EMS therefore evolves from reactive rescuers into proactive water safety champions.
FAQ: EMS and Water-Related Emergencies
What should EMS teams do differently in saltwater versus freshwater drownings?
Rescuers anticipate greater pulmonary edema in saltwater cases due to osmotic shifts. They secure airways fast and monitor saturation throughout transport.
How does cold-water immersion affect resuscitation chances?
Cold water slows metabolic demands, often extending viable resuscitation windows beyond typical expectations. Crews warm patients aggressively before considering termination protocols.
Are there protocols for working with volunteer water-rescue teams?
Agencies establish joint drills and credential reviews to ensure consistent skill levels. Unified incident command structures streamline responsibilities during real operations.
When should EMS recommend transport after a near-drowning if the patient appears stable?
Medics advise transport whenever submersion lasted longer than seconds or symptoms appeared. Hospital observation catches delayed complications like secondary drowning.
3 Practical Tips for EMS Teams Handling Water Emergencies
- Pack a waterproof rescue kit that includes suction, airway devices, and hypothermia wraps in one grab-and-go bag.
- Conduct monthly shoreline drills that measure throw-bag accuracy, role communication, and patient extrication speed.
- Preprogram radios with marine, lifeguard, and helicopter frequencies to eliminate scrambling during multi-agency incidents. Store laminated rip-current and spinal-immobilization cues inside every ambulance for quick on-scene reference. Review equipment batteries and strap integrity after each mission, ensuring readiness for the next call.
Where Readiness Meets Reality: Why Proactive Planning Saves Lives
Water emergencies escalate rapidly, yet practiced crews turn frightening scenes into coordinated rescues. Quarterly drills, strategic equipment placement, and community outreach together forge resilient systems. Public trust grows when residents see EMS acting as educators rather than last-chance heroes. Survivors and families remember clear communication and compassionate care long after beaches reopen. Leaders who invest in prevention programs observe fewer tragedies and stronger responder morale. Continual improvement ensures every splash of summer fun remains memorable for joy, not for loss.

Lisa VanderMeulen brings over 15 years of field experience as a licensed paramedic and firefighter in Florida. She currently serves as a Lieutenant with the Lehigh Acres Fire Control & Rescue District and as Dean of Ricky Rescue Training Academy, where she oversees curriculum development for EMT and fire service education.
Lisa holds an Associate of Science in Emergency Medical Services Technology from Florida SouthWestern State College and advanced certifications from the Florida Bureau of Fire Standards & Training, including Fire Officer II, Fire Instructor II, and Incident Safety Officer. Her licensure as a paramedic is backed by the Florida Department of Health.
In addition to her teaching and command roles, she actively serves on safety committees, community outreach programs like Fire Prevention Week and Pink Heals, and holds leadership positions within IAFF Local 1826.

